
Regorafenib Becomes First FDA-Approved Drug for Liver Cancer in Nearly a Decade
May 24, 2017, by NCI Staff
On April 27, the Food and Drug Administration (FDA) approved regorafenib (Stivarga®) for some patients with hepatocellular carcinoma (HCC), the most common form of liver cancer. The expanded approval is for the treatment of patients with HCC whose tumors have stopped responding to a similar targeted therapy, sorafenib (Nexavar®).
The action by FDA makes regorafenib—which is also approved for use in some patients with some gastrointestinal cancers—the first new therapy approved for liver cancer in nearly a decade.
In November 2007, sorafenib became the first-ever FDA-approved drug for liver cancer. The approval was for patients with HCC that cannot be removed by surgery.
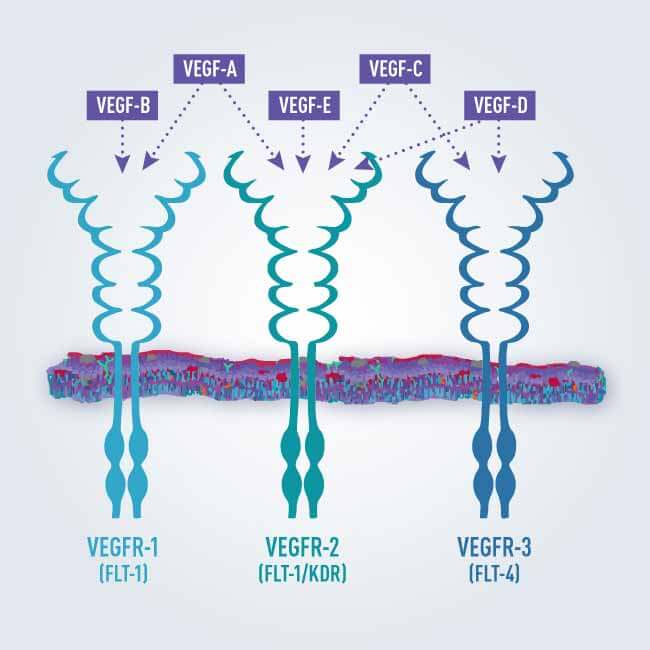
Both regorafenib and sorafenib are kinaseinhibitors, drugs that block enzymes that control cell division and proliferation. In fact, “the drug and the mechanism of action of regorafenib are almost identical to sorafenib,” said Tim Greten, M.D., of the Thoracic and Gastrointestinal Oncology Branch of NCI’s Center for Cancer Research. “So it’s not something that’s completely new.”
In the time since sorafenib was approved there have been several phase III trials for treatments of liver cancers that have had negative results, Dr. Greten said.
“So having a positive trial result with an FDA approval is a significant advancement in the field,” he explained.
Clinical Trial Results
The approval was based on the results of a phase III clinical trial of 573 patients whose HCC had progressed after treatment with sorafenib. The patients were randomly assigned to receive either regorafenib or, because no systemic treatments have been available for such patients, a placebo.
Median overall survival in the trial was 10.6 months for patients who received regorafenib, compared with 7.8 months for patients in the placebo group. Median progression-free survival was 3.1 months and 1.5 months, respectively. The overall response rate, or percentage of patients whose tumors shrank at least partially after treatment, was 11% for the patients who took regorafenib and 4% for those who took the placebo.
The most common severe adverse events for patients who took regorafenib included hypertension, hand-foot skin reaction, and fatigue. Regorafenib was approved with a black box warning for liver damage (hepatotoxicity), and FDA warned the drug is associated with other serious side effects, including infections, heavy bleeding, and wound healing complications.
“The increase in overall survival by 3 months is an important finding for these patients,” said Dr. Greten, who was not involved in the study that led to the approval. Unfortunately, participating centers were not required to collect tumor biopsies, he continued, “which would have been helpful for follow-up studies and to understand what’s happening on a molecular level, to see if there are biomarkers for response.”
Patients in this trial are a select group, Dr. Greten cautioned, because they could tolerate sorafenib’s side effects.
“We know that sorafenib is not very well tolerated by many patients,” he said. “So now there is the question of how many patients outside of a clinical trial will benefit from regorafenib, because some of them won’t be able to tolerate first-line treatment with sorafenib.”
Testing Other Treatments
Other potential treatments for liver cancer may be on the horizon. Several immunotherapy agents, for example, are being tested in clinical trials.
In March 2017, Dr. Greten and his colleagues published positive results from a clinical study in patients with advanced HCC that tested whether the immune checkpoint inhibitor tremelimumab could be safely combined with radiofrequency ablation, which is used in some patients with small liver tumors. The researchers think that ablation may be able to trigger the immune system to target tumor cells and that checkpoint inhibitors could enhance this effect.
Other checkpoint inhibitors, including nivolumab (Opdivo®), are being tested in clinical trials for patients with advanced HCC who had previously received sorafenib.
One phase III trial is also being conducted that is testing nivolumab against sorafenib as a first-line treatment in patients with advanced HCC.






















.png)











No hay comentarios:
Publicar un comentario