
For HPV-Positive Women, Test Can Guide Cervical Cancer Screening Follow-Up
October 11, 2018, by NCI Staff
A new test can help to improve the clinical management of women who screen positive for human papillomavirus (HPV) infection in routine cervical cancer screening, an NCI-led study has shown.
The test, called p16/Ki-67 dual stain, more accurately predicted whether an HPV-positive woman would go on to develop cervical precancer within 5 years, compared to a Pap test—the current standard for managing HPV-positive women.
As HPV testing becomes more central to cervical cancer screening, “the challenge is how to best manage, or triage, HPV-positive women,” said senior investigator Nicolas Wentzensen, M.D., Ph.D., of NCI’s Division of Cancer Epidemiology and Genetics (DCEG).
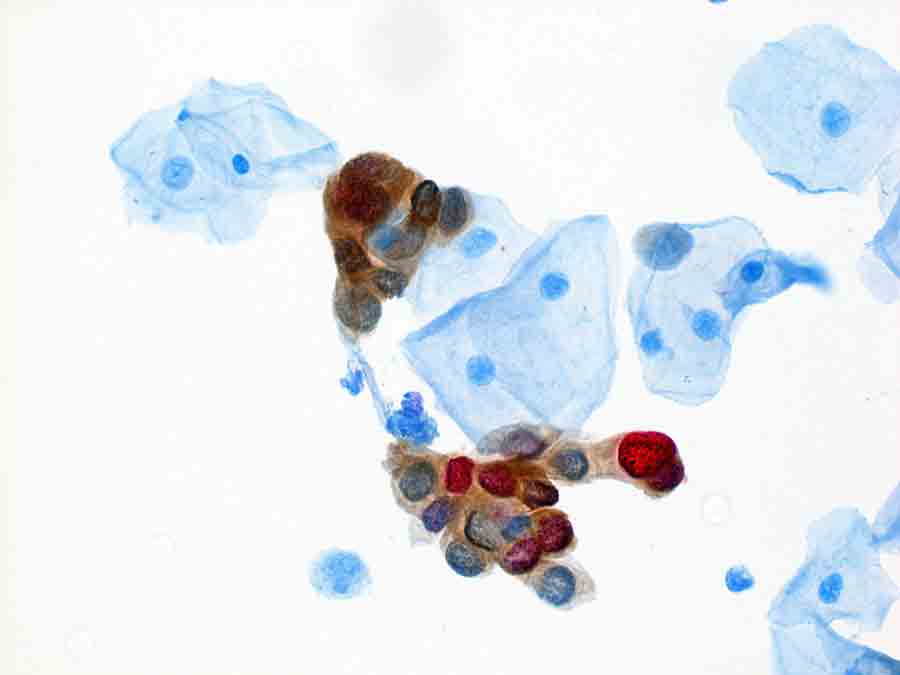
Dual stain testing measures the presence of two specific proteins, p16 and Ki-67, in Pap test samples. Previous studies have suggested that the combination of these two markers is better at identifying HPV-positive women who have precancers than Pap testing.
The study’s lead investigator, Megan Clarke, Ph.D., M.H.S., also of DCEG, said that it addresses a critical question: “how often and at what time interval should HPV-positive women who test negative with dual stain come back for repeat screening?”
In the prospective study, HPV-positive women who had a negative result on the dual-stain test had a low risk of developing cervical precancer over the ensuing 5 years, the researchers reported October 11 in JAMA Oncology. These women, they concluded, can safely wait 3 years before undergoing their next round of screening.
“This is a very important study,” said Mark Stoler, M.D., associate director of Surgical Pathology and Cytopathology at the University of Virginia School of Medicine. It’s the first study performed in the United States, Dr. Stoler continued, “that really provides the assurance that [dual stain] is a better triage test” than the Pap test.
Cervical Cancer Screening in the US
There are many sexually transmitted HPV types, approximately 12 of which are known to cause cervical and several other cancers. HPV infections are very common, but most are controlled by the immune system and do not lead to cancer. When an infection persists for many years, however, it can cause cells to undergo changes and may ultimately become cancer.
Testing cervical cells for HPV infections is now recommended as a standard way to screen for those early changes, so researchers are searching for ways to distinguish between HPV infections that are likely to cause cancer—and therefore require follow-up procedures—and infections that can be safely monitored. Follow-up procedures include colposcopy, during which biopsies of abnormal areas in the cervix are taken. Biopsy-confirmed precancers can then be removed by one of several different methods.
Current guidelines for cervical cancer screening recommend one of three approaches: the Pap test alone, the HPV test alone, or a combination of the two—known as an HPV/Pap cotest. According to the US Preventive Services Task Force (USPSTF), women age 30 to 65 years at average risk of cervical cancer can be safely screened with an HPV test or HPV/Pap cotest every 5 years.
Historically, the Pap test greatly reduced the incidence of cervical cancer in all countries where screening was implemented. The addition of the HPV test further improved the accuracy of screening. But this approach has some limitations.
For example, women who test positive for HPV and who have minor abnormalities on a Pap test are usually referred for immediate colposcopy. But only a small percentage of abnormalities turn out to be cervical precancer or cancer, meaning that most of these women may have received a colposcopy that was unnecessary, Dr. Wentzensen explained.
Because of these limitations, “there is a big effort to find better markers that allow us to triage HPV-positive women more efficiently,” said Dr. Wentzensen.
The dual-stain approach has been under study for more than a decade, Dr. Stoler said. The expression of p16 is strongly linked with HPV infection, and Ki-67 is used as a biomarker for the rapid cell division seen in precancers and cancer.
In terms of potential triage approaches for HPV-positive women, dual-stain testing “is probably the most advanced method available,” added Dr. Clarke. This new study adds to that body of evidence, she said.
Searching for a Better Triage Test for HPV-Positive Women
To conduct the study, the investigators followed 1,549 women aged 30 or older who had tested positive for HPV while undergoing routine HPV/Pap cotesting at Kaiser Permanente Northern California between January and May 2012.
Women with a normal, or negative, Pap test result were recommended to repeat the cotest in 1 year, while women with an abnormal, or positive, Pap test result were referred for immediate colposcopy. Colposcopy results can reveal a range of disease states, including normal, low-grade to high-grade precancer, and cancer.
Dual-stain testing was performed on participants’ Pap test samples at the time of enrollment, and the women were then followed for 5 years.
Overall, 46% of women in the study had a positive dual-stain test and 51% had a positive Pap test. Compared with women with normal Pap results, more women with severely abnormal Pap test results had a positive dual-stain test, the researchers found.
The same was true for the biopsy results: Over the 5-year study period, 77% of women found to have a high-grade precancer and 91% found to have cancer had a positive dual-stain test.
The team also found that, compared with Pap test results, dual-stain test results were far more indicative of the 5-year risk of cervical precancer.
For example, women with a negative dual-stain test result had a lower risk of developing cervical precancer within 5 years, compared to women with a negative Pap test. This means that a negative dual-stain test result gives greater reassurance than a negative Pap test result that precancer won’t develop during the ensuing 5 years, Dr. Wentzensen explained.
Conversely, women with a positive dual-stain test result had a higher risk of developing cervical precancer over the next 5 years than women with a positive Pap test result. That finding, together with the lower positivity of dual stain, suggests that using the dual stain test to triage HPV-positive women might lead to fewer unnecessary colposcopies, Dr. Clarke noted.
Based on the 5-year risks of cervical precancer, the researchers determined that women with a negative dual-stain result can wait 3 years before being screened again.
The ability of the dual stain test to improve on the sensitivity of the Pap test (i.e., better identifying women with a higher risk of having precancer) and its specificity (i.e., better at identifying those with a low risk) is impressive, Dr. Stoler said.
“It’s very hard to have a test that improves sensitivity and specificity, but dual stain does it because of the biology behind the development of the test,” he said.
Learning More About Dual Stain
The dual stain test is already being marketed and used in several countries, including Canada, Europe, and Australia, Dr. Stoler said. The clinical trial that would form the basis of clearance of the dual stain test by the Food and Drug Administration for its use in the United States is currently ongoing, he added.
In the future, HPV testing followed by dual stain for primary cervical cancer screening may be a more efficient alternative to HPV/Pap cotesting, Drs. Wentzensen and Clarke said.
The manufacturer of the dual stain test is analyzing the development of cervical precancer in HPV-positive women who have a positive test result from either dual stain or Pap in an ongoing study. In addition, Dr. Wentzensen and his colleagues are investigating the results of dual stain testing in a large population of women, including many who are HPV-negative.
“I think there will be sufficient data to change practice based on these observational studies,” said Dr. Wentzensen.
And the test may soon have other attractive qualities, the investigators noted. A major advantage of the dual stain test, said Dr. Wentzensen, is that abnormal cells are highlighted with a colored stain and are therefore easier to detect and quantify.
“Currently, the dual stain test is evaluated manually, but we are working on an automated evaluation of this assay and we have exciting results,” he added. Automation of the dual-stain test would enhance its reliability and make it easier to use, he said.


































No hay comentarios:
Publicar un comentario