
What are CAR T cells?
Utilizing the immune system for advanced cancer treatment has shown remarkable potential in recent years. One of the most promising immunological approaches to cancer therapy is the employment of CAR T cells.
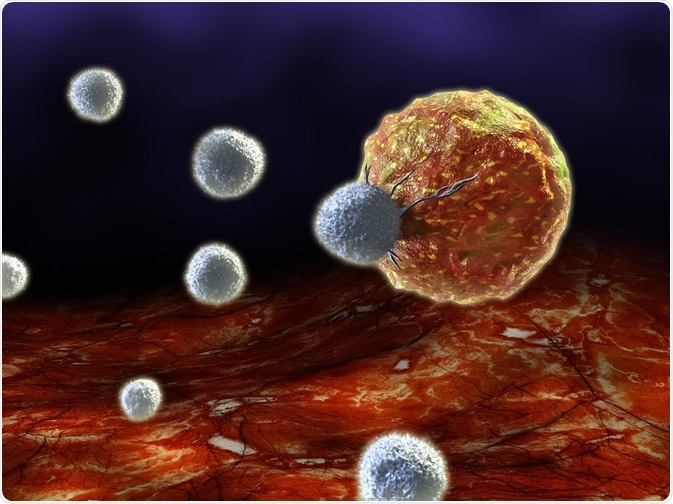
Credit: Andrea Danti/Shutterstock.com
Chimeric antigen receptors (CAR) are engineered T cell receptors that redirect T cells to recognize and destroy cancer cell targets. CAR T cells are referred to as chimeric because they are engineered from parts that originate within different sources.
Clinical efficacy has been demonstrated in hematologic malignancies with two CAR T cell therapies approved by the FDA in 2017 for the treatment of acute lymphoblastic leukemia in children and advanced lymphomas in adults. Nonetheless, research into other potential treatments, particularly for solid tumors, is ongoing and future enhancements to vector choice and the avoidance of side effects are required.
Structure of CAR T cells
The basic structure of a chimeric antigen receptor consists of the ectodomain, transmembrane domain, and endodomain. The ectodomain is the section of membrane protein that is external to the cytoplasm and open to extracellular space. The signal peptide or single-chain variable fragment (scFv) in the ectodomain directs the nascent protein into the endoplasmic reticulum.
The antigen recognition domain of the CAR functions by recognizing antigens through high-affinity ligands and is connected to the transmembrane by a spacer. The transmembrane domain provides stability for the whole chimeric antigen receptor through a hydrophobic alpha helix structure. The endodomain is where receptors cluster to activate an antigen recognition signal that is then transmitted to the T cell.
Engineering CAR T cells for cancer therapy
CAR T cell therapy requires the collection of T cells from the blood of the patient or donor. A vector is then used to genetically engineer the T cells to produce the surface receptors that allow the T cell to recognize and bind to specific antigens on cancer cells.
Viruses are the major vector for the delivery of required genes because of their high transfer efficiency, wide availability, and the short time needed to reach a large numbers of T cells. A challenge to the employment of viral vectors is the potential introduction of DNA mutations as the vector DNA is integrated into the genome of the host cell. Currently, several long-term studies are monitoring for delayed adverse events which may be caused by viral vectors.
For this reason, non-viral vectors, including liposomes and molecular conjugates, are also being investigated . The engineered T cells are then multiplied within the laboratory before being reinfused into the patient. The CAR T cells are able to further multiply within the body while destroying the targeted cancer cells that display the specific surface antigen.
Current limitations of CAR T cells for cancer therapy
Though CAR T cell therapy has shown clinical efficacy in treating hematologic malignancies, the results from solid tumors were less successful. The reported antigen loss in tumor cells lead to reduced number of unique antigens and the immune-suppressive microenvironment of solid tumors. Combining CAR T cells with other effector molecules may prove to be a superior strategy for the treatment of solid tumors.
Another major limitation to CAR T cell therapy is the potential induction of cytokine release syndrome. T cells release cytokines which act as messengers to direct immune response. During cytokine release syndrome, the rapid release of inflammatory cytokines and the subsequent activation of more white blood cells cause severe and sometimes fatal symptoms, such as high fever, low blood pressure, and seizures.
This side effect is an expected outcome of active CAR T cells working within the body. Current CAR T cell treatments manage cytokine release syndrome through standard support therapies which include steroids.
Reviewed by P Surat, PhD
Sources:
- National Cancer Institute: CAR T Cells: Engineering Patients’ Immune Cells to Treat Their Cancers.
- Maus, M.V. et al. 2016. An MHC-restricted antibody-based chimeric antigen receptor requires TCR-like affinity to maintain antigen specificity, Molecular Therapy Oncolytics, 3:16023.
- Zhang, C. et al. 2017. Engineering CAR-T cells, Biomarker Research, 5:22.
- D’Aloia, M.M. et al. 2018. CAR-T cells: the long and winding road to solid tumors, Cell Death and Disease, 9:282.
- Bonifant, C.L. et al. 2016. Toxicity and management in CAR T-cell therapy, Molecular Therapy Oncolytics, 3: 16011.
Further Reading
Last Updated: Apr 2, 2018





















.jpg)












No hay comentarios:
Publicar un comentario