
Study reveals subtypes of lymphoma
At a Glance
- Researchers identified genetic subtypes of diffuse large B-cell lymphoma, the most common type of lymphoma.
- They also showed that these subtypes can be used to predict treatment response. The findings may help doctors better tailor treatments.

Lymphoma is cancer that begins in a kind of white blood cell known as a lymphocyte, usually a B cell. There are many types of lymphoma, and they receive different kinds of treatment. The most common type is diffuse large B-cell lymphoma (DLBCL). Although DLBCL is usually a fast-growing cancer, some people can be treated successfully with chemotherapy and a monoclonal antibody. However, for unknown reasons everyone with DLBCL doesn’t respond to this treatment.
Several years ago, researchers defined two major subgroups of DLBCL. The groups arise from different B cells and have different patterns of gene activity. They also found that the likelihood that treatment would cure the disease varied by subgroup. About 40% of people with activated B-cell-like (ABC) DLBCL live for 5 years after treatment, while about 75% of people with germinal center B-cell-like (GCB) DLBCL live that long.
An international research team led by Dr. Louis M. Staudt at NIH’s National Cancer Institute (NCI) set out to find whether the tumor’s genetics could explain different treatment responses. The scientists analyzed DLBCL’s genetic features, divided tumors into subtypes, and compared treatment responses for the subtypes. The results were published on April 12, 2018, in the New England Journal of Medicine.
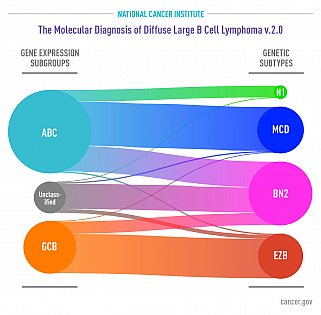
The research team analyzed genomic alterations and gene expression in tumor samples from 574 people with DLBCL. They identified four prominent subtypes that each share a group of genetic aberrations. People with two of the subtypes, called BN2 and EZB, respond well to treatment. People with the other two, called MCD and N1, don’t.
These genetic subtypes aren’t simply a refinement of the previously defined subgroups; some can be found in both the ABC and GCB subgroups. This refined genetic understanding of DLBCL can help doctors find the right treatments for their patients.
“Before, even with our most advanced molecular diagnosis, we would have said all ABC tumors are the ‘bad’ type and they need to be treated aggressively,” Staudt explains. “Now we can implement this kind of classification and say that even if a patient has the ‘bad’ ABC type, they have the ‘good’ genetic type, BN2. So there’s a much better chance of chemotherapy curing the disease.”
“This refined molecular classification will be instrumental in predicting prognosis and tailoring therapy for patients with DLBCL going forward,” adds NCI Director Dr. Ned Sharpless.
Related Links
- Tumor DNA in Blood Reveals Lymphoma Progression
- Study Suggests New Approaches to Burkitt Lymphoma
- Mutations Contribute to Type of Non-Hodgkin Lymphoma
- Gene Activity Can Predict Survival Rates of Patients with Lymphoma
- Gene Expression Profiling Distinguishes Lymphomas
- Cancer Care Gets Personal: How Tumor Treatments Are Changing
- Lymphoma
References: Genetics and Pathogenesis of Diffuse Large B-Cell Lymphoma. Schmitz R, Wright GW, Huang DW, Johnson CA, Phelan JD, Wang JQ, Roulland S, Kasbekar M, Young RM, Shaffer AL, Hodson DJ, Xiao W, Yu X, Yang Y, Zhao H, Xu W, Liu X, Zhou B, Du W, Chan WC, Jaffe ES, Gascoyne RD, Connors JM, Campo E, Lopez-Guillermo A, Rosenwald A, Ott G, Delabie J, Rimsza LM, Tay Kuang Wei K, Zelenetz AD, Leonard JP, Bartlett NL, Tran B, Shetty J, Zhao Y, Soppet DR, Pittaluga S, Wilson WH, Staudt LM. N Engl J Med. 2018 Apr 12;378(15):1396-1407. doi: 10.1056/NEJMoa1801445. PMID: 29641966.
Funding: NIH’s Intramural Research Program and National Cancer Institute (NCI); Oxford–Cambridge Scholars Program; Dr. Mildred Scheel Stiftung für Krebsforschung (Deutsche Krebshilfe); Washington University in St. Louis Medical Scientist Training Program; and Kay Kendall Leukaemia Fund.





















.png)












No hay comentarios:
Publicar un comentario