
Improving the Diagnosis of Cardiac Sarcoidosis
 Thought LeadersDr. Nadera SweissProfessor of RheumatologyThe University of Illinois at Chicago
Thought LeadersDr. Nadera SweissProfessor of RheumatologyThe University of Illinois at ChicagoAn interview with Dr. Nadera Sweiss, MD, FACR, conducted by Kate Anderton, BSc
What is cardiac sarcoidosis?
Cardiac sarcoidosis is an inflammatory disease of the heart that results in various clinical manifestations. It is characterized by the presence of granulomas in the heart, which may be the first manifestation of sarcoidosis.
 Credit: Liya Graphics/Shutterstock.com
Credit: Liya Graphics/Shutterstock.comHow often is sarcoidosis present in other areas of the body in addition to the heart?
Sarcoidosis as an inflammatory disease that commonly involves various organs in the body, basically from head to toe. Patients quite often show signs of sarcoidosis in the brain, lungs, heart, liver and joints.
The commonest organ is the lung, but we are not sure how common this is in relation to cardiac sarcoidosis. There haven’t been many studies to give us a clear answer about the exact prevalence and the occurrence outside the heart. This is often because we're comparing various studies from various parts of the world, so the numbers vary quite a bit.
So, the exact answer to your question is we really do not know. It depends on the organ, the center, where do you practice, and what kind of specialty you do, and how extensively do you look to find sarcoidosis in other organs.
How is cardiac sarcoidosis currently diagnosed?
The guidelines have changed over the past couple of years and are likely to change again but currently, the gold standard for accurately diagnosing cardiac sarcoidosis is the presence of signs and symptoms, as well as evidence from a cardiac PET/CT scan, and/or a cardiac MRI.
It is likely that in the future, there will be hybrid machines that will combine both. But the way we most often diagnose it at our center is using a cardiac PET/CT scan. This is because many patients have metal in their body, such as a pacemaker or defibrillator, which are not compatible with MRI. There are now MRI machines that are compatible with metal, and newer devices that are MRI-friendly, but not every institution or patient has these.
In patients where we cannot perform a cardiac MRI, we do the cardiac FDG PET/CT but in an ideal world, we'd love to be able to do both tests together.
What is FDG?
FDG is an abbreviation for Fludeoxyglucose, a glucose analog that we give to patients prior to a PET scan. It is taken up by organs with a high demand for glucose, such as the heart or cancer cells, instead of physiologic glucose. It acts as a radioactive dye that allows us to visualize abnormalities and diagnose sarcoidosis in the heart, for example.
Why is a high-fat, low-sugar diet recommended when diagnosing cardiac sarcoidosis via FDG-PET?
If you do not deplete the body of glucose a few days before the test, the results may be affected by the normal physiologic uptake of glucose in the heart. This could make it look like as if the patient has sarcoid in the heart, when in reality, the observations are due to poor preparation. This is known as a false positive result.
Most centers recommend a high-fat, low-sugar diet for at least 24 hours before an FDG-PET. However, this technique hasn’t been validated. We currently use the 72 hour preparation based on our recent study utilizing this technique, and found that the three-day diet leads to much clearer images. Ho
Why is it important to combine FDG-PET scanning with CT scanning?
Computer tomography (CT) scanning is a good way of detecting lesions in the heart, such as granulomas in cardiac sarcoidosis. It helps us to see the size and location of any lesions but doesn’t tell you anything about the activity of the lesion.
FDG-PET can tell you whether the lesion is active or inactive, whether there is physiologic uptake of the glucose in the sarcoid, or whether it is something else entirely. When you combine these tests, you’re able to see the physiologic and pathologic uptake of glucose in the tissue, in addition to evaluating the size of the nodule or the inflammation in the lung.
Having said that, we sometimes carry out the FDH-PET with a perfusion study, which allows us to make sure that if we can see something in the heart, we don't misdiagnose it as sarcoid when it is, for example, due to a decrease in blood flow to the heart, or another issue.
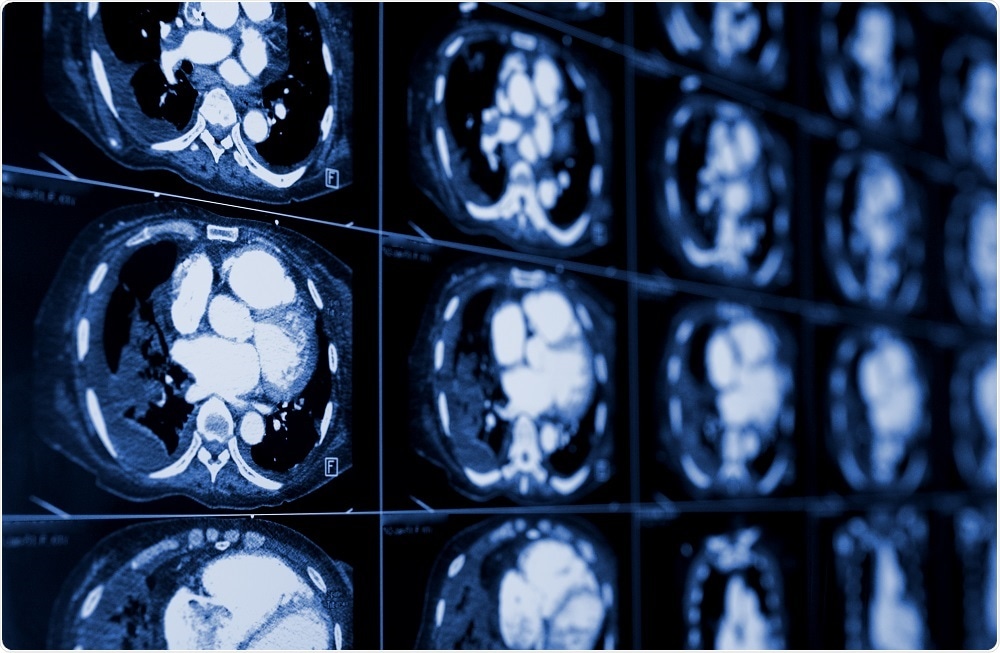 Credit: sfam_photo/Shutterstock.com
Credit: sfam_photo/Shutterstock.comPlease describe your recent research into the diagnosis of sarcoidosis.
As previously mentioned, we published in January 2017 where we looked at the use of an FDG-PET/CT scan to diagnose cardiac sarcoidosis.
Our hypothesis was that the myocardial physiologic uptake of FDG is unpredictable, so if we put patients on a 72 hour pre-test high-fat, high protein, and very low carbohydrate diet, which we referred to as HFHPVLC, it could suppress the physiologic uptake of the FDG, and thus help us identify active cardiac sarcoidosis.
Although it was a retrospective study, we had a large number of patients; 215 patients underwent an FDG PET/CT test. The results suggested that if patients are subjected to the pro-longed 72 hour diet, the FDG-PET/CT scan was more sensitive and was a more accurate method of diagnosing active cardiac sarcoidosis than the 24 hour diet previously used.
Our study changed standard practice around the world, with most institutions now using the 3 day diet. However, I believe a larger study is needed, to validate our results fully. We then looked at using a PET scan to stage the disease. We wanted to find out whether we could use the PET scan of the heart to diagnose sarcoidosis outside the heart.
We took the same patients as our previous study who had been diagnosed with cardiac sarcoidosis and looked at the images again. We tried to define sarcoidosis outside the heart, and to our surprise, we found 20 scans that were positive for cardiac sarcoid among the 188 patients (around 40%).
This number needs to be validated, as I suspect that it will vary from 20% to 60%, depending on the center. So, the answer to our research question was, yes, the PET scan useful to diagnose at sarcoidosis outside the heart, but it needs validation.
What projects are you currently working on?
We were recently awarded a grant from the National Institute of Health. The principal investigators on the grant are Dr. Patricia Finn, the Earle M. Bane Professor of Medicine and Head of the UIC Department of Medicine, and Dr. David Perkins, Professor of Medicine, Surgery, and Bioengineering at UIC. I am one of the co-investigators. It will be used to fund research into the microbiome and the host’s immune response in sarcoidosis.
Our hypothesis is that the microbiome is altered in patients with sarcoidosis, affecting their immune responses. We will hopefully correlate our results with PET scan images as well, in order to improve diagnoses.
On the clinical side, we are current conducting some clinical trials into new therapies for sarcoidosis. Our main area of interest is cardiac sarcoidosis and over the next year, we hope to study the macrophages and T cells in cardiac sarcoidosis, and how they relate to other types of sarcoidosis.
We’re going to look at lung sarcoid, heart sarcoid, kidney sarcoid, and most likely liver sarcoid too, and compare the results to normal controls, to try to further our understanding of the pathophysiology and the immunology of cardiac sarcoidosis.
Where can readers find more information?
About Dr. Nadera Sweiss
 Dr. Nadera Sweiss is a specialist in rheumatology, the study of chronic and acute conditions that cause inflammation and sees a wide variety of patients with autoimmune diseases.
Dr. Nadera Sweiss is a specialist in rheumatology, the study of chronic and acute conditions that cause inflammation and sees a wide variety of patients with autoimmune diseases.Dr. Sweiss directs the Bernie Mac Sarcoidosis Translational Advanced Research (STAR) Center, which she helped establish together with the Bernie Mac Foundation at the University of Illinois Hospital & Health Sciences System in 2012.
The STAR Center conducts research into new treatments for sarcoidosis, and also provides clinical services for patients with sarcoidosis. She is also director of the UI Health Cold Hand Clinic.
Sweiss is a principal investigator of numerous clinical trials that focus on finding treatments for sarcoidosis, scleroderma, Raynaud’s phenomenon and rheumatoid arthritis when these disorders do not respond to traditional therapies.





















.png)












No hay comentarios:
Publicar un comentario