
There is hope

Medically assisted treatment for opioid use can break the cycle of addiction.
The United States is in the middle of an opioid overdose epidemic, according to the Centers for Disease Control and Prevention, which calculates that more than 350,000 deaths are attributed to opioid overdoses nationwide since 1999. The military is at the forefront of efforts to help curb those numbers through its expansion of medically assisted treatment, also known as MAT.
Vice Adm. Raquel C. Bono, director of the Defense Health Agency, reported to the House Armed Services Committee last month that the military’s rate of deadly opiate overdoses is a quarter of the national average, according to House transcripts. Dr. Fuad Issa, chief of the implementation section at the DHA Psychological Health Center of Excellence, said the availability of MAT has a lot to do with breaking the cycle of addiction.
In 2016, the Department of Defense expanded the availability of MAT as part of the TRICARE benefit, with the goal of increasing successful treatment and reducing the number of overdoses and deaths due to opiate abuse, said DHA clinical psychologist and senior policy analyst Dr. Krystyna Bienia.
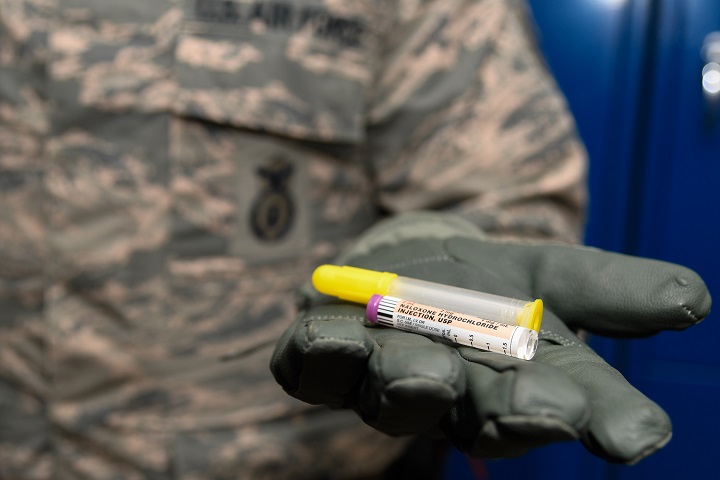
“Drugs like methadone, naltrexone, and buprenorphine as a medically assisted treatment plan relieve withdrawal symptoms and psychological cravings that make opiate addiction so hard to overcome,” she said. “Used correctly, and in conjunction with psychotherapy, support, and counseling, they can help users overcome the addiction to opioids.”
The Substance Abuse and Mental Health Services Administration points out that the benefits of MAT include not only curbing withdrawal symptoms and preventing cravings, but also providing medical supervision. MAT works to normalize brain chemistry, block the euphoric effects of opioids (which include prescription drugs such as hydrocodone and oxycodone), and stabilize body functions without the negative effects of the abused drug. MAT has proven to be clinically effective and significantly reduces the need for inpatient detoxification. Bienia notes that MAT provides a comprehensive, individually tailored program of medication and behavioral therapy.
Yet some MAT medications have challenges of their own. Methadone, for example, doesn’t produce euphoria; rather, it tricks addicts into thinking they’re getting the opiate, according to the National Institute on Drug Abuse. Methadone works by changing how the brain and nervous system respond to pain. But according to Issa, methadone itself can be addictive.
That’s why Navy Capt. Edward Simmer, psychiatrist and chief clinical officer for TRICARE, believes it’s important to realize that the medication is only one component of the treatment plan. He suggests part of his patients’ treatment is going to 12-step programs such as Narcotics Anonymous, and including other community support.
“There’s a large social component to drug use,” Simmer said. “Relapses are often caused by being around others who use drugs, or stresses associated with drug use. Therefore, successful treatment requires eliminating these triggers to the greatest extent possible.”
Bienia explained that the duration of MAT depends on the patient. “After months or a year or more of treatment, the medication can be gradually reduced and eventually stopped … but in some cases [it] has to be taken for a lifetime,” she said.
Issa noted that in the past, opiate users had to get their medication at a special dosing site, but today, a prescription for drugs effective in alleviating opiate withdrawal symptoms, such as the combination of buprenorphine and naloxone, can be filled at a local pharmacy. The 2016 TRICARE Mental Health and Substance Use Final Rule allows TRICARE-authorized physicians to provide office-based opioid treatment.
Issa said he believes this may be making a difference, noting that in addition to TRICARE changes, DoD has been training medical providers on the risks of opioids. The number of DoD opioid prescriptions dropped by 56 percent between 2013 and 2017.
According to Bono’s testimony to the House committee, less than 1 percent of active-duty service members are abusing or addicted to opioids.
In 2017, the DHA Psychological Health Center of Excellence, along with the Medical Directorate - National Capital Region, trained 192 physicians to prescribe MAT, and more nurse practitioners are being added this year to expand the network and coverage of MAT providers, said Issa.
“Beating an addiction is a drastic change in someone’s life, but treatment works,” said Simmer. “People do overcome addiction when everyone works together. There is hope.”
Life without liquor
Article
6/29/2018

One service member’s story of how he overcame a drinking problem
Progress in preventing opioid abuse, more needs to be done
Article
6/26/2018
The Military Health System has a shared responsibility in addressing the nation’s opioid epidemic
Going the distance runs in the family
Article
6/14/2018

For this father/daughter team, running, and the Marine Corps principles that carry them, are in their blood
DHA PI 6025.04: Pain Management and Opioid Safety in the MHS
Policy
The purpose of our MHS Pain Management Campaign is to enable Clinical Communities to provide evidence-based pain management guided by clinical practice guidelines (CPGs): effectively treat acute and chronic pain; promote non-pharmacologic treatment; prevent acute pain from becoming chronic; and minimize use of opioids with appropriate prescribing only when indicated. The Pain Management Clinical Support Service achieves these ends through clinical improvements in pain care, clinician and patient education, and research. This Defense Health Agency-Procedural Instruction (DHA-PI) is a dual effort between the Pain Management Clinical Support Service and the Clinical Communities to achieve our stated purpose through implementation of the MHS Stepped Care Model.
- Identification #: DHA PI 6025.04
- Date: 6/8/2018
- Type: DHA Procedural Instruction
- Topics: TRICARE Pharmacy Program | Substance Abuse
Breaking down anxiety one fear at a time
Article
6/5/2018

Generalized anxiety, panic disorder, and anxiety related to PTSD are common disorders. In fact, an estimated 31 percent of U.S. adults experience anxiety at some point in their lives; one marine discusses his journey.
Assess your mental wellness during Mental Health Awareness Month
Article
5/25/2018

TRICARE provides mental health services for you and your family at all times
TRICARE Mental Health
Video
5/24/2018

Watch this video to learn more about the mental health care benefits TRICARE provides
Breaking down the image: Mental health
Article
5/22/2018

May has been National Mental Health Month since 1949
Years in the making: How the risk for Alzheimer’s disease can be reduced
Article
5/18/2018

About 3 million new cases of Alzheimer’s Disease, the most common form of dementia, are diagnosed every year. Experts say lifestyle modifications can help prevent this disease.
Making behavioral health care easy
Article
5/11/2018

Embedded behavioral health teams let service members easily access behavioral health care right in their unit areas
Ready, set, focus: Finding calm in a storm through the power of breathing
Article
4/23/2018

‘Mindful minutes’ and deep breathing help on the job, airmen say
Military providers seek tailored approach to treating PTSD
Article
3/14/2018

New tool reviews, monitors provider prescribing habits
Traumatic Brain Injury and the Art of Paddling
Article
3/7/2018

A U.S. Army veteran’s recipe for embracing life after several TBIs
New DoD educational podcast series promotes better health
Article
3/5/2018
The instructional podcasts highlight health technology and offer tips, tools and techniques to help improve the lives of those in the military community
Rocky and Elmo want providers to "Watch. Ask. Share."
Article
2/12/2018

How DHA teamed with Sesame Street to help care for military families


































No hay comentarios:
Publicar un comentario