
I learned how to retrain my brain to manage chronic pain

Retired Navy Senior Chief Petty Officer Jim Wilt
Approximately 50 million Americans live with chronic pain, according to a report from the Centers for Disease Control and Prevention, and many of those suffering have served in the armed forces. The National Health Interview Survey found that military veterans are more likely to experience chronic pain than people who've never worn the uniform.
Pain can take many forms: sharp, dull, strong, mild, intermittent, constant. Acute pain is sudden, usually brought on by illness or injury. With time, it resolves. Chronic pain is the result of increased sensitivity of the nerves. And it can be unrelenting in terms of frequency and severity. Chronic pain may even lead to anxiety, depression, and a reduced quality of life.
According to the CDC, many people rely on prescription medications to manage their pain. I did, too, after breaking my back during a training accident early in my Navy career as a parachute rigger and jumper. I spent some time recuperating but once back on the job, I was still hurting. There were many days I'd wake up, take medication to mask the pain, and then push through the day.
Other mission-related injuries exacerbated the pain. I worked with my doctors to adjust medications and dosages. But at some point, I realized it didn't make sense for me to continue living life this way. The meds were clouding my mind, preventing me from being fully present for my family.
Moreover, they were ultimately adding to the problem. Let's say my back hurt. I'd take a couple of pills and then, feeling no pain, continue working past the point when I should have stopped. The overexertion would leave me almost completely debilitated for a day or two afterward, when the pain medication wore off. And the body can develop a tolerance to medication over time, according to the National Institute on Drug Abuse
I put off back surgery because of potential risks, including paralysis and infections. Several years after retiring and well into my second career as a senior scientist for Naval Air Systems Command, I had a spinal fusion procedure. After recuperating, I approached my doctors about learning how to retrain my brain so that I could taper off the meds and take a holistic approach to managing my pain. Tools for retraining the brain include physical therapy, yoga, and dietary changes.
Pain is your body's way of telling you to throttle back. I've learned to listen to and heed that signal. Instead of taking meds and continuing with what I was doing, I stop. The work will still be there tomorrow. You just pick up and do it in stages, rather than try to knock it all out in one day.
Additionally, I look for other ways to feel better. I practice yoga and meditation, and I do a stretching routine I learned in the military. I also follow a healthy diet and make sure I stay hydrated.
Today, I'm not completely pain-free. I'm usually a 6 on the Defense and Veterans Pain Rating Scale, which health care providers use to assess pain intensity as well as how pain impacts daily activities, including work and sleep. A "6" means my pain is difficult to ignore. It can cause me to avoid usual weekend activities, such as splitting logs, mowing the lawn, and tending to my gardens. Still, I feel better overall now that I no longer take prescription pain medications. I've regained the ability to feel real, authentic emotions.
I understand that for some people, it may not be wise or safe to eliminate prescription pain medications altogether. But if you're looking for a lifestyle change – and it is, indeed, a lifestyle change – talk to your health care provider about options for pain management that don't rely on meds. Be open and honest about how you're feeling physically as well as emotionally, and bring your family members in on the conversation as well. You need not be alone in this.
Opioid Abuse and Non-Opiate Pain Management
Congressional Testimony
7/12/2019
H.R. 6157, HAC Report for FY 2019, 115-769, Pg. 298
Acute vs. Chronic Pain
Infographic
6/6/2019

This infographic describes the difference between acute pain and chronic pain
Living with Pain? Retrain Your Brain
Infographic
6/6/2019

This infographic describes ways to retrain the brain's reaction to pain.
Breaking the pain cycle
Article
4/9/2019

Live in agony or risk addiction? MHS pain management initiatives offer options
MHS Pain Management 2019
Fact Sheet
4/3/2019
This document provides images for a pain rating scale, from 0 to 10, along with supplemental questions.
Drug-monitoring innovations help providers help their patients
Article
8/6/2018
Focus is on management of pain and PTSD
Progress in preventing opioid abuse, more needs to be done
Article
6/26/2018
The Military Health System has a shared responsibility in addressing the nation’s opioid epidemic
HIMSS session includes update on MHS Opioid Registry
Article
3/12/2018

Shared registry for DoD, VA is in development
Battlefield acupuncture shows promising results downrange
Article
12/27/2017

Research has shown how beneficial battlefield acupuncture can be in combat settings
Acupuncture: Ancient technique complements modern medicine
Article
11/29/2017

Procedure has a role in easing pain, advocates say
Burn Center offers new pain management approach for patients
Article
11/8/2017

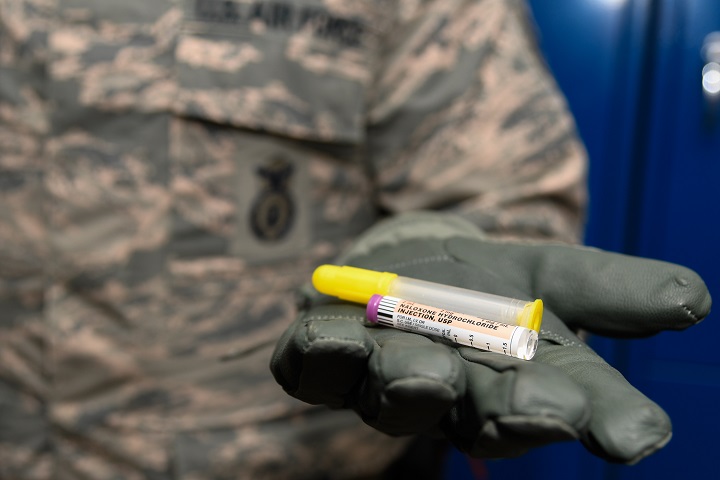
The pain medication is managed with the placement of an intrathecal catheter and infusion of preservative-free morphine





















.png)












No hay comentarios:
Publicar un comentario