
HPV Vaccination Linked to Decreased Oral HPV Infections
June 5, 2017, by NCI Staff
New study results suggest that vaccination against the human papillomavirus (HPV) may sharply reduce oral HPV infections that are a major risk factor for oropharyngeal cancer, a type of head and neck cancer.
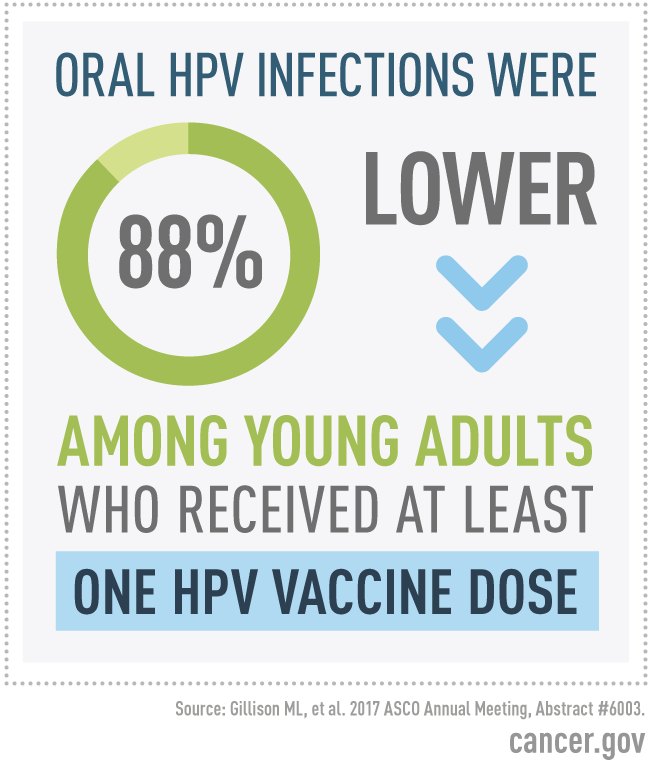
The study of more than 2,600 young adults in the United States found that the prevalence of oral infection with four HPV types, including two high-risk, or cancer-causing, types, was 88% lower in those who reported receiving at least one dose of an HPV vaccine than in those who said they were not vaccinated.
About 70% of oropharyngeal cancers are caused by high-risk HPV infection, and the incidence of HPV-positive oropharyngeal cancer has been increasing in the United States in recent decades. In the United States, more than half of oropharyngeal cancers are linked to a single high-risk HPV type, HPV 16, which is one of the types covered by Food and Drug Administration (FDA)-approved HPV vaccines.
“In an unvaccinated population, we would estimate that about a million young adults would have an oral HPV infection by one of these vaccine HPV types. If they had all been vaccinated, we could have prevented almost 900,000 of those infections,” said senior study author Maura Gillison, M.D., Ph.D., of the University of Texas MD Anderson Cancer Center.
Dr. Gillison presented the new findings at a May 17 press briefing ahead of the 2017 annual American Society of Clinical Oncology (ASCO) meeting, held June 2–6 in Chicago.
A Rapidly Rising Cancer
Oropharyngeal cancer “is the fastest-rising cancer among young white men in the United States,” said Dr. Gillison, who was at Ohio State University when she conducted the study.
“The HPV types that cause oropharyngeal cancers are primarily transmitted through sexual contact,” explained lead study author Anil Chaturvedi, Ph.D., of NCI’s Division of Cancer Epidemiology and Genetics. The increased incidence of oropharyngeal cancers in white men has been linked to changes in sexual behaviors from the 1950s through the 1970s, he said. The exact reasons for the greater increase in oropharynx cancer incidence in men versus women are still unclear, Dr. Chaturvedi added.
Clinical trials have shown that FDA-approved HPV vaccines can prevent anogenital HPV infections and precancerous lesions that lead to HPV-associated cancers, including cervical and anal cancer. However, Dr. Gillison said, the potential impact of current HPV vaccines on oral HPV infections that lead to cancer has not yet been rigorously tested in clinical trials, and thus the vaccines are not specifically approved for preventing cancers of the oropharynx.
From 2006 through 2014, most HPV-vaccinated individuals in the United States received Gardasil®, an HPV vaccine that protects against infection with HPV types 6, 11, 16, and 18. In January 2015, FDA approved an updated HPV vaccine, Gardasil 9®, that protects against five additional HPV types.
Looking for a Link
To investigate the relationship between HPV vaccination and oral HPV infection, the researchers analyzed data for 2,627 young adults who participated in NHANES, a national survey that assesses the health of a representative slice of the US population.
Drs. Gillison, Chaturvedi, and their colleagues restricted their analysis to NHANES data from 2011 to 2014, focusing on 18- to 33-year-old men and women “because they were the first group [in the United States] to receive the vaccine,” Dr. Gillison said.
In the United States, routine vaccination against HPV, which causes nearly all cervical cancers, has been recommended since mid-2006 for 11- to 12-year-old girls and for females up to age 26 who have not previously been vaccinated. HPV vaccination has been recommended for males ages 9–26 since 2009.
The researchers analyzed mouth rinse samples (containing oral cells) from all study participants for the presence of 37 HPV types, including types 6, 11, 16, and 18, which are covered by Gardasil, Dr. Gillison said.
The prevalence of oral infections with these four HPV types was 1.61% in unvaccinated young adults versus 0.11% in vaccinated young adults—an 88% reduction in HPV prevalence with vaccination. Among men, the prevalence of oral infection with the four HPV types was 2.1% in unvaccinated individuals and 0.0% in vaccinated individuals.
By contrast, the prevalence of oral infection with 33 HPV types not covered by the vaccine was 4.0% in vaccinated groups and 4.7% in non-vaccinated groups, the researchers found, a difference that was not considered to be statistically meaningful.
Vaccination rates were low overall, with only 29.2% of women and 6.9% of men in the study population reporting having received at least one dose of an HPV vaccine before age 26.
Prevention Potential
Although the self-reported vaccination rates in this study were low, Dr. Gillison said, “there is considerable optimism because more recent data indicate that [roughly] 60% of girls and 50% of boys under age 18 have received more than one HPV vaccine dose.”
“HPV vaccines are already strongly recommended for cancer prevention,” Dr. Gillison continued. “Parents who choose to have their children vaccinated against HPV should realize that the vaccine may provide additional benefits, such as preventing oral HPV infections linked to oral cancers.”
However, she and Dr. Chaturvedi noted, only a randomized clinical trial that follows people over time could definitively show a cause and effect relationship between HPV vaccination and a lasting reduction of high-risk oral HPV infections, which experts agree is a more meaningful indicator of vaccine effectiveness.
In July 2013, NCI researchers and their collaborators reported findings from the NCI-sponsored HPV Vaccine Trial in Costa Rica that suggested that HPV vaccination can reduce oral HPV infections in women.
“Our study builds on those results by showing a reduction in oral HPV prevalence in vaccinated men, the group that bears the greatest burden of HPV-associated oropharynx cancers,” Dr. Chaturvedi said.





















.jpg)












No hay comentarios:
Publicar un comentario