
Volume 24, Number 10—October 2018
Dispatch
Acute Encephalitis with Atypical Presentation of Rubella in Family Cluster, India
On This Page
Sumit D. Bharadwaj1, Rima R. Sahay1, Pragya D. Yadav, Sara Dhanawade, Atanu Basu, Virendra K. Meena, Suji George, Rekha Damle, and Gajanan N. Sapkal
Abstract
We report 3 atypical rubella cases in a family cluster in India. The index case-patient showed only mild febrile illness, whereas the other 2 patients showed acute encephalitis and died of the disease. We confirmed rubella in the index and third cases using next-generation sequencing and IgM.
Rubella is usually considered a mild viral infection. Approximately 25%–50% of infections are asymptomatic (1). Differential diagnosis of viral acute encephalitis syndrome (AES) caused by rubella, herpes simplex virus, measles, varicella zoster virus, and Epstein–Barr virus infections can be accomplished through the unique presentation of rash in each case. Rubella typically presents as fever with rash and is mostly diagnosed clinically, but rubella leading to fatal AES is rare (1/6,000 cases) (2). A cluster of rubella-associated encephalitis has been reported from Japan (3) and rubella encephalitis without rash from Tunisia (4).
We report on rubella in 3 unvaccinated siblings in India. We investigated this family cluster at the request of the treating physician in August 2017, on the eighth day postinfection of the index case-patient.
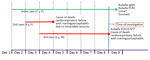
Figure. Timeline of clinical events for 3 siblings infected with rubella and encephalitis, India. *Negative for Japanese encephalitis virus, Chandipura virus, dengue virus, West Nile virus, enterovirus, and herpes simplex virus. CSF,...
The affected family belonged to a lower-middle income group in a village in Maharashtra, India. The father worked as a ward attendant at a hospital, and the mother was a homemaker. There were 3 children in the family; the index rubella case-patient was a 7-year-old girl, who recovered following a mild febrile illness. The 2 other siblings, an 8-year-old girl and a 2-year-old boy, died of acute encephalitis within 4 days of onset of disease (Figure). No history of similar illness in the neighborhood, travel history, or visitors were reported. There was also no history of consumption of fruits or accidental ingestion of any toxic drugs or pesticides before symptom onset. Nutritional status for all children was normal for height, weight, and body mass index.
The index case-patient developed a low-grade intermittent fever; her temperature rose in the evening. The fever subsided within 2 days after the patient took acetaminophen. She had not been immunized against rubella. Her throat was uncongested and there were no rashes or mucocutaneous lesions. Systematic examination revealed no abnormalities. Biochemical tests were normal. Tests for dengue virus and malarial parasites were negative. The child recovered without any sequelae. The investigating team examined her on the eighth day following onset of symptoms.
Two days following onset of illness in the index case-patient, her 8-year-old sister developed a high-grade fever and eye pain. There was no history of rash or mucocutaneous lesions. On day 2 of her illness, she had multiple episodes of convulsions with nonprojectile vomiting and was admitted to a hospital. On day 3, she was put on a mechanical ventilator, but she died that day. The cause of death was cardiorespiratory failure with meningoencephalitis due to intractable seizures. This child had not been immunized for rubella; no clinical samples were available to test.
One day after the onset of fever in the second patient, her 2-year-old brother developed a mild fever with no rash or mucocutaneous lesions. His intermittent fever subsided after he took acetaminophen. Two days later, he developed a high-grade fever with convulsions and nonprojectile vomiting. He became semiconscious, with decerebrated rigidity. He became comatose and was put on mechanical ventilation on day 4 of his illness. Plantar reflex was absent, and deep tendon reflexes were diminished. No cardiovascular system abnormality was noted. His chest was clear, with no wheeze or stridor. Abdominal examination revealed no notable organomegaly. The child received antimicrobial drugs, phenytoin, mannitol, and acyclovir. He died on day 5 of his illness. Details from the medical records for the second and third case-patients are provided in Technical Appendix 1 Table 1.
We tested serum and urine samples from the index case-patient and serum, urine, and cerebrospinal fluid (CSF) samples from the third case-patient for Japanese encephalitis virus (5), West Nile virus (6), Chandipura virus (7), and enteroviruses (8) using real-time quantitative reverse transcription PCR (qRT-PCR); for dengue, chikungunya, and Zika viruses using CDC Trioplex qRT-PCR; and for rubella using RT-PCR (9). We further used quantitative PCR to test for varicella zoster virus DNA (10) and PCR for herpes simplex virus 1 (Genekam Biotechnology, Duisburg, Germany, No. K091). We also tested samples for rubella IgM and IgG using a Siemens Healthcare Kit (Siemens, Erlangen, Germany). We extracted RNA and DNA using a QIAAmp total nucleic acid extraction kit (QIAGEN, Hilden, Germany).
We obtained a rubella nested PCR product of 185 bases from a CSF sample from the third case-patient; no amplification was obtained from serum and urine, so we used the CSF sample for next-generation sequencing (11).We tested serum samples from close contacts of the index and third case-patients for the presence of rubella IgM and IgG (Table 1; Technical Appendix 2). We prepared the RNA library following the defined protocol (12) using a TruSeq Stranded mRNA Library preparation kit (Illumina, San Diego, CA, USA); quantified it using a KAPA Library Quantification Kit (Roche, Indianapolis, IN, USA); and loaded it on an Illumina Miniseq NGS platform. We imported raw RNA data of 147 MB in CLC Genomics Workbench software (QIAGEN) for further analysis. We assembled the RNA data using de novo and reference assembly methods and obtained 1.9 million reads with an average length of 138 bp. From the total read, 0.57% mapped to the reference genome (GenBank accession no. JN635296) with an average length of 123 bp. De novo assembly of reads gave 86 contigs with an average length of 1,281 bp. Reference mapping led to a ≈8 kb region (4.5 kb of nonstructural protein [NSP], 3 kb of structural protein [SP], and 0.5 kb in both NSP and SP regions) that was broken intermittently (GenBank accession nos. MG987207.1 for NSP and MG987208.1 for SP) (Technical Appendix 1 Figure 1). We used a 732-bp E1 gene sequence to identify the rubella genotype (Technical Appendix 1 Figure 1). The phylogenetic tree that we constructed revealed that this virus belongs to rubella genotype 2B (Table 2; Technical Appendix 1 Figure 2).
Rubella encephalitis without identification of typical rubella rash is rarely reported. In the cluster we describe, the parents were asymptomatic and positive for anti-rubella IgG when tested on the eighth day from the onset of symptoms in the index case-patient. The rubella IgM equivocal status of the father suggests that he could be a possible source of infection to the family. His occupation as a hospital ward attendant also indicates a possibility of infection either through respiratory secretions or by contact with an infectious agent on his body or on items carried to and from his workplace. In rubella, neurologic symptoms most often occur 1–6 days after the onset of the exanthem (13). In this cluster, rapid disease progression meant the second and third case-patients died within 4 days of illness onset. The index case-patient tested positive for rubella IgM on the eighth day postinfection and the third case-patient tested positive for rubella IgM on the fifth day postinfection, but their specimens were negative for IgG, suggesting that the children were not immunized and had not had any past rubella infection. A serum sample from the index case-patient from the 14th day postinfection was IgG positive. Through epidemiologic linkage, the causative agent in the second case may be similar to that for the other cases.
In conclusion, rubella encephalitis can present without rash. Rubella virus infection should be considered in the differential diagnosis of AES in unvaccinated children.
Dr. Bhardwaj and Dr. Sahay are medical scientists at the National Institute of Virology, Pune, India, and are trained in clinical and field epidemiology. Their research areas include respiratory illness of viral origin and emerging and reemerging viral infections as well as clinical and epidemiological investigation of disease outbreaks.
Acknowledgment
We gratefully acknowledge the guidance and technical expertise provided by D.T. Mourya and B.V. Tandale throughout this investigation. We also acknowledge support rendered by Pradeep Awate and Milind Pore, by Bipin Telekar and Shiv Shankar for assistance and outbreak logistics preparation, and by all the staff of Virus Research and Diagnostic Laboratories, Japanese Encephalitis, and BioSafety Level 4 laboratory for the technical support. We acknowledge the Centers for Disease Control and Prevention, Atlanta, GA, USA, for generously providing the Trioplex reagents.
References
- Prober CG. Central nervous system infections. In: Behrman RE, Kliegman RM, Jenson HB, editors. Nelson textbook of pediatrics. Philadelphia: W.B. Saunders, 2004. p. 2038–47.
- Paret G, Bilori B, Vardi A, Barzilay A, Barzilay Z. [Rubella encephalitis]. Harefuah. 1993;125:410–1, 447.PubMed
- Ishikawa T, Asano Y, Morishima T, Nagashima M, Sobue G, Watanabe K, et al. Epidemiology of acute childhood encephalitis: Aichi Prefecture, Japan, 1984–90. Brain Dev. 1993;15:192–7. https://dx.doi.org/10.1016/0387-7604(93)90064-F
- Sapkal GN, Wairagkar NS, Ayachit VM, Bondre VP, Gore MM. Detection and isolation of Japanese encephalitis virus from blood clots collected during the acute phase of infection. Am J Trop Med Hyg. 2007;77:1139–45. https://dx.doi.org/10.4269/ajtmh.2007.77.1139PubMed
- Sapkal GN, Bondre VP, Fulmali PV, Patil P, Gopalkrishna V, Dadhania V, et al. Enteroviruses in patients with acute encephalitis, Uttar Pradesh, India. Emerg Infect Dis. 2009;15:295–8. https://dx.doi.org/10.3201/eid1502.080865
- Bosma TJ, Corbett KM, O’Shea S, Banatvala JE, Best JM. PCR for detection of rubella virus RNA in clinical samples. J Clin Microbiol. 1995;33:1075–9.PubMed
- World Health Organization. Standardization of the nomenclature for genetic characteristics of wild- type rubella viruses [cited 2017 Sep 13]. http://www.who.int/immunization/monitoring_surveillance/burden/laboratory/Rubella_nomemclature_report.pdf?ua=1
Figure
Tables
Cite This ArticleOriginal Publication Date: 8/28/2018
1These authors contributed equally to this article.


































No hay comentarios:
Publicar un comentario