
Addressing Antimicrobial Resistance Through Industry
 insights from industryGary Cohen & Steve ConlyBecton, Dickinson & Co
insights from industryGary Cohen & Steve ConlyBecton, Dickinson & CoWhat is antimicrobial resistance (AMR)? What impact does it have on a patient’s treatment?
Gary: Antimicrobial resistance (AMR) is a term used to describe a loss of effectivity of commonly used drugs, like antibiotics or antifungals, against pathogenic organisms.

Credit: Sirirat/Shutterstock.com
AMR has a fundamental impact on patient care from several perspectives. One is that patients are routinely being prescribed antibiotics for non-bacterial infections such as the flu, where they are not effective in combating the underlying condition.
The effect they have can do more harm than good. Antibiotics have detrimental effects on the normal microflora of the body, which may actually be suppressing the viral infection.
If you disrupt the delicate ecosystem, you not only lose this protection, you can also encounter situations where resistant bacteria survive the antibiotics and take over the patient’s microbiome, a condition that can potentially be deadly.
Steve: In countries where patients must pay for treatment, AMR increases costs dramatically. Given the economic status of the world we currently live in, mounting costs for patients and the healthcare industry are of great concern.
How does antimicrobial resistance spread?
Gary: The first route of exposure is through skin. Most often, patients carry resistant organisms on their skin, but are not infected with a resistant bacterial strain.
These patients will go into hospital for an invasive procedure such as surgery or insertion of a catheter, and the resistant organism will spread to a vulnerable part of the body, resulting in a resistant infection.
Resistant organisms also exist in the community. For example, a young woman who received treatment for an infection, picked it up while scuba diving on her honeymoon.
She was misdiagnosed and prescribed a broad-spectrum antibiotic that killed off much of her healthy bacteria, resulting in two life or death bouts in the ICU. Luckily, she recovered well and was able to go home, but she is now more susceptible than ever to future infections.
It is also an outcome of the misuse of antibiotics. Using antibiotics in food, for example, creates a selective environment for resistant bacterial strains to thrive.
In addition, active ingredients used in antibiotic manufacturing can contaminate way streams, increasing exposure of organisms in the environment to antibiotics. Finally, giving patients the wrong antibiotic, or patients not finishing a course of antibiotics, can contribute to the development of resistance.
How are antimicrobial resistant diseases diagnosed? Are there any barriers to diagnosis?
Steve: The diagnosis of bacterial infections, specifically resistant ones, is done through diagnostic testing. There are multiple technologies in use now, the uses of which depend on the particular symptoms the patient is exhibiting, the severity of their condition and the country in which the test is being carried out.
The simplest way to prevent AMR infections is using point-of-care testing in primary care, before any prescriptions are written. These tests can help distinguish between a viral and bacterial infection; and that’s the first question to answer.
The next test, which is performed in a laboratory, will identify the causative strain, which can be worked out using traditional methods or molecular methods, which are more common these days. The final test is the susceptibility test, to work out which interventions will actually kill, or treat, the infection.
The barriers to diagnosis depend on the location and setting, as many physicians do not have access to sufficient laboratory resources, especially in developing countries. In the UK and the US, access is not the biggest barrier, and resistance rates are lower because of that.
Gary: Even where the instruments and tests exist, and in theory access in not an issue, there is a lack of utilization. Tests are not being used properly or as frequently as they need to be used. This is a recognized problem even in the most developed countries; their labs will likely have the instruments but are not carrying out the full testing protocols.
It’s very common for physicians to treat and prescribe antibiotics empirically, based on the symptoms that they visually observe. Another barrier is time. The current tests can take as much as two to three days to get all the answers.
We, and everyone else, would like to be able to reduce the amount of time it takes to confirm a diagnosis using laboratory tests and that is evident by the huge focus on innovation at the moment. Point of care testing can help, but today there are only two countries in the world that routinely use flu testing at the primary care level, the U.S. and Japan.
Are there any alternatives to broad-spectrum antibiotics?
Gary: For many years, clinicians were taught to ‘throw the kitchen sink’ at the infection, meaning they should always use a broad-spectrum antibiotic. The reasoning behind this is that because it's not so targeted, it will kill off everything, including the primary infection. However, what was overlooked, and people are just starting to realize, is that healthy bacteria are critical to our immune system and thus, fighting infections.
Broad spectrum antibiotics not only kill the pathogenic bacteria, but also the healthy bacteria that constitute the microbiome. In addition, the use of a broad-spectrum antibiotic in resistant infections, like MRSA or C. difficile, creates a selective environment for the pathogenic bacteria to thrive, and the patient is more at risk than ever.
The dilemma a clinician faces, especially when prescribing, should not be underestimated. There are infections that do not require treatment and those that require fast treatment, such as sepsis, which is blood stream infection. Physicians must be able to decide based on their experience, their observation, and diagnostic testing, what may require fast intervention and what does not.
Another issue is that patients go into primary care expecting treatment. This is a problem all over the world and causes physicians to feel pressure to prescribe an oral antibiotic, or in some countries an injection to treat the patient. Often, the patient’s immune system could have fought off the infection after a few days.
It's not up to us to decide what the clinical practice should be, but the awareness of the different options and the knowledge about the use of the best tools is critical in this situation. The use of more targeted antibiotics, as well as improvements in diagnostics are all critical factors in the fight against AMR.
Steve: At present, there are no alternatives to antibiotics that are routinely available to clinicians. The best way of preventing antimicrobial resistant infections is through reducing the amount of antibiotics used. Scientists are also working on new vaccines.
Newer technologies are being investigated, but these are still very early in terms of their technical development and availability. One example is the new pneumococcal vaccine, and even more well-known ones like the flu vaccine.
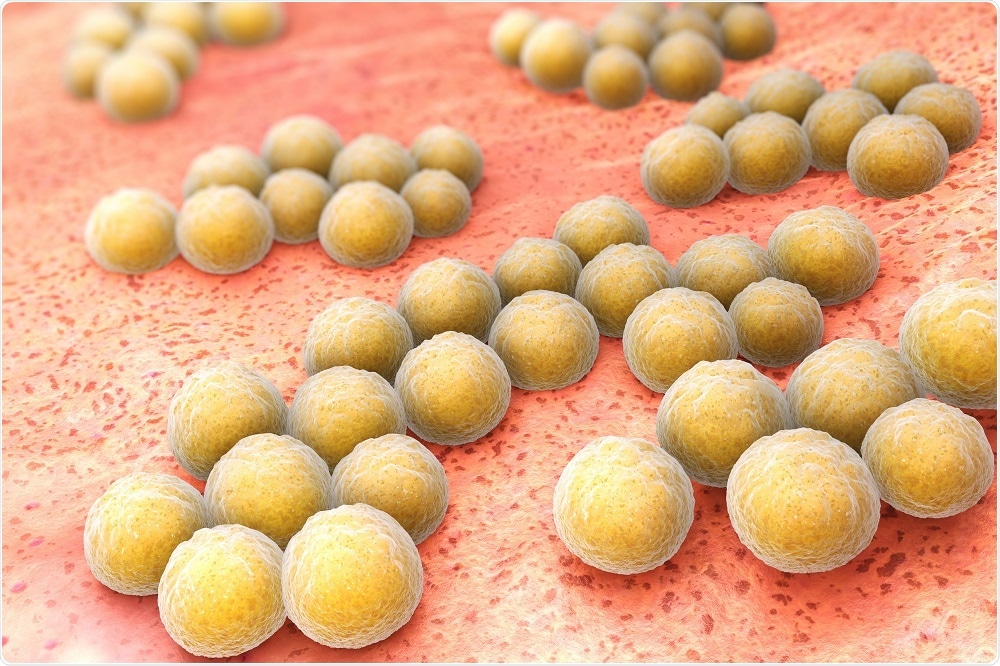
Methicillin-Resistant Staphylococcus aureus (MRSA) Credit: Tatiana Shepeleva/Shutterstock.com
What is the AMR (Antimicrobial Resistance) Alliance and what is its mission?
Gary: Becton Dickinson (BD) is a 121-year-old established company, with much of the company's development historically around the area of infection prevention and control and the origins of use of diagnostic medicine, particularly microbiology. We're also a commercial supplier of medical devices and diagnostic testing instruments.
The AMR Industry Alliance is a group that was initially formed by pharmaceutical companies and then joined by diagnostic companies. We are working to mobilize the capabilities of the private sector of industry to combat AMR. Everyone understands that this can't be done without the private sector, so it is great that professionals from industries ranging from manufacturers to private health providers can come together to combat the spread of AMR.
We partner across sectors to collaborate to combine the capabilities of the public sector, non-government organizations, health agencies, and the private sector, to tackle major health problems worldwide. For AMR, we are bringing those capabilities to the forefront, because this is one of the biggest human health issues we are facing right now.
What steps are being taken to reduce the spread of antimicrobial resistance?
Gary: There are two practices that are particularly important to reduce the spread of AMR in the human health sector (excluding food production, agriculture and antibiotic production).
One of these is practicing effective infection prevention and control. This means that if a patient comes into the hospital with an infectious disease that may be caused by a potentially resistant organism, they are identified from the beginning, isolated and treated before they can spread it to other patients.
This extends to other areas such as pre-surgical preparation procedures for invasive surgeries such as insertion of a catheter, and basics like hand washing and the proper use of gloves.
The second area is antimicrobial stewardship; a process to ensure that antimicrobials, especially antibiotics, are being used properly. Diagnostics play a critical role, yet most antimicrobial stewardship programs don't focus that much on diagnostics but rather on limiting the use of antibiotics.
This approach can be a double-edged sword because there are certain cases where you do have to use antibiotics and you don't want to deny a patient in need access to them.
Wanting to address this issue, we recently entered into a collaboration with the London School of Hygiene and Tropical Medicine to develop a new antimicrobial stewardship program, particularly focused on the use of diagnostics.
We are also mobilizing a broad-based awareness and coalition-building campaign around AMR called the Antimicrobial Resistance Fighter Campaign. It's unusual that we're doing this because we're taking on a role that the public sector would normally take on, but since it wasn't happening, we thought it would make sense for us to mobilize it and then make it available broadly.
It's not a BD branded program, we're making it available to any health facility, organization, leader, professional society, and government organization that wants to engage. We have 30 world leading organizations already on board, all the way through to individual patients, or families of patients that have been impacted by AMR.
At the rate we're going, we're expecting that there will be hundreds of organizations engaged by summer 2018, all of whom will be unified under the umbrella of ‘I'm a Resistance Fighter!’.
The AMR Resistance Fighter Campaign will work to create a message in a consistent format that features the organization, the leader, the patient, or the family, and their story about how they are taking personal responsibility to combat AMR. Through this, we hope to raise awareness of the issue and get more people engaged.
How are the public and private sectors working together to address antimicrobial resistance?
Gary: Fortunately, AMR is something that everybody realizes is a huge issue, and are all willing to work together to mitigate. The door for collaboration is open, and we’re putting more emphasis than ever on the capabilities that industry can provide.
We’re working to improve training and pushing to align this with guidelines, policies and the use of diagnostics. People know that the correct identification and treatment of resistant infections will reduce costs, but they don’t realize that it will save money, so it will pay for the investment in new technologies.
Other than antibioitics, what else should be addressed to help reduce the prevalence of antimicrobial resistance?
Gary: Everybody understands a pill, you feel sick, you have a fever, the doctor gives you a pill, and you get better. It's such a simple concept even though in practice it's not anywhere near that simple.
Most patients are not aware of what happens in a laboratory, therefore, they're not thinking to go into a physician’s office and say, "Might this be a resistant infection? Have you done the proper tests? Could it be sepsis? Which could be life threatening in a manner of days."
Even among health leaders who may have some understanding of diagnostics in the laboratory, there's an underestimation about how important this is.
A recent AMR review, led by Jim O'Neal, called for mandatory diagnostic testing in developed countries before antibiotics would be prescribed, which is very different from what is done today. The number one message for us is that you can't control or combat AMR without the use of diagnostics.
Where can readers find more information?
About Steve Conly
 Steve is the Vice President of Microbiology within Diagnostic Systems at BD. He is responsible for leading the Blood Culture, TB, Industrial Microbiology, Lab Automation and Informatics franchises. Steve joined BD in 2010 with the acquisition of Dynacon’s Lab Automation business.
Steve is the Vice President of Microbiology within Diagnostic Systems at BD. He is responsible for leading the Blood Culture, TB, Industrial Microbiology, Lab Automation and Informatics franchises. Steve joined BD in 2010 with the acquisition of Dynacon’s Lab Automation business.Steve earned his Bachelor of Arts and Sciences degree from McGill University in Montreal where he majored in Biomedical Sciences and Economics.
About Gary Cohen
 Gary Cohen is Executive Vice President and President of Global Health and Development at BD (Becton, Dickinson & Co), a global medical technology company. He joined BD in 1983 and has served as an executive officer since 1996.
Gary Cohen is Executive Vice President and President of Global Health and Development at BD (Becton, Dickinson & Co), a global medical technology company. He joined BD in 1983 and has served as an executive officer since 1996.In addition to serving as board co-chair of GBCHealth, he is a board director of the Perrigo Company, CDC Foundation, UNICEF USA, the Federal Drug Agents Foundation and the End Violence Partnership. He also serves as chair of the CDC/Corporate Roundtable on Global Health Threats and as an advisor on the Scientific Advisory Board of Grand Challenges Canada.
Mr. Cohen is among the foremost private sector leaders working in collaboration with the public and non-profit sectors to advance global public health. His team collaborate with international agencies, governments and non-government organizations to address global health needs such strengthening health systems, addressing infectious and non-communicable diseases, reducing maternal and newborn mortality, combating antimicrobial resistance and improving safety for health workers and patients.





















.png)












No hay comentarios:
Publicar un comentario