
Black women are 'twice as likely to die' from aggressive uterine cancer
Researchers at the National Cancer Institute (NCI) have published a new study showing that incidence rates for aggressive subtypes of uterine cancer in the US rose rapidly in women aged between 30 and 79 from the years 2000 to 2015.
The study also highlights racial disparities between the incidence and survival rates of aggressive cancers in non-Hispanic black women compared to other racial and ethnic groups.
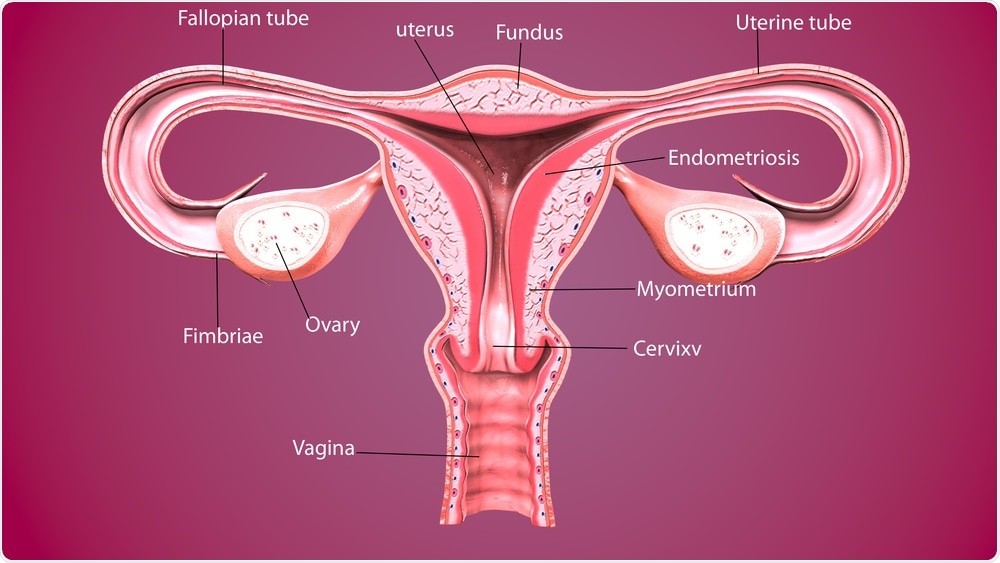 Life science | Shutterstock
Life science | ShutterstockThe study was published in the Journal of Clinical Oncology on May 22nd 2019. Its purpose was to evaluate “recent trends in hysterectomy-corrected rates by race and ethnicity and histologic subtype,” as well as to estimate discrepancies in survival rates relative to race, ethnicity, subtype, and cancer stage.
The research involved population data from the NCI Surveillance, Epidemiology, and End Results (SEER) database and assessed the incidence rates for women as a whole, breaking the demographic groups down further into race and ethnic groups, geographic region, and histologic subtypes. These are subtypes of uterine cancer which are differentiated by how the tissue looks under microscopic study.
Trends within these groups were then charted, revealing concerning results.
The researchers also corrected for hysterectomy prevalence with data from the Behavioral Risk Factor Surveillance System. This was to account for women who had undergone a hysterectomy and who were no longer at risk from developing uterine cancer, a factor that many other uterine cancer incidence studies had not accounted for in the past.
The results were ‘very concerning’
Dr. Megan Clarke, the lead author of the study and a postdoctoral fellow in the NCI Division of Cancer Epidemiology and Genetics, spoke on the benefits of correcting for hysterectomy-corrected uterine cancer.
"Incidence rates of uterine cancer have been rising, and there have been previous reports of racial differences in incidence and survival rates, with disparities observed for non-Hispanic black women.
"But few recent studies have corrected for hysterectomy, which can vary by race and ethnicity and by region. Correcting for hysterectomy prevalence gives us a more accurate picture of trends in overall incidence, as well as rates by race and ethnicity."
The results of the NCI study found that among women as a whole, the incidence rates of uterine cancer corrected by hysterectomy had increased by 1 percent per year from 2003 to 2015.
While incidence rates in white women have risen, this increase has been slower than that of women from other ethnic and racial groups. Incidence rates in black women were higher than in white women in 2007, and remained higher from 2011 to 2015.
The study describes this difference between ethnic and racial groups as “profound”.
Uterine cancer is the most common and second most deadly gynecologic cancer in the US. It is estimated there were 63,230 new cases of uterine cancer and 11,350 deaths caused by the disease in 2018.
These rates have been projected to increase substantially in the future.
“These trends and predictions have been largely attributed to increasing obesity rates, population aging, and decreased use of combined menopausal hormone therapy,” the study reveals.
The incidence rates of endometrioid subtypes remained stable in non-Hispanic white women during the duration of the study but increased in other racial and ethnic groups.
Conversely, the incidence rates of aggressive, non-endometrioid subtypes significantly increased in all racial and ethnic groups with an overall increase of 2.9 percent per year from 2000 to 2015.
25.9 per 100,000 black women had significantly higher rates of non-endometrioid subtypes, compared to 11.4 white women per 100,000, 10.1 Hispanic women, and 7.5 Asian/Pacific Islanders.
Although uterine cancer with endometrioid histology has a good prognosis overall, uterine cancer with non-endometrioid histology is a more aggressive form of uterine cancer and has a far worse prognosis.
Black women are ‘twice as likely to die’
It is black women that are more likely to be diagnosed with aggressive non-endometrioid subtypes, despite having lower uterine cancer incidence rates in the past.
Black women have also been “twice as likely to die as a result of uterine cancer compared with white women, making this one of the largest racial disparities observed for any cancer type.”
However, the increase in non-endometrioid subtypes of uterine cancer may not be explained by the increasing incidence in obesity or changes in hormone replacement therapy during the menopause, with these lifestyle factors being associated more strongly with the less aggressive endometrioid subtypes of uterine cancer.
The study shows that black women had “substantially lower 5-year relative survival, irrespective of stage at diagnosis or histologic subtype,” with the authors suggesting that a combination of “biologic and care-related factors” may be contributing to this worrying trend.
Another interesting finding from the study is that increases in recent years have been caused by increasing rates of aggressive nonendometrioid histologic subtypes of uterine cancer in all racial and ethnic groups.
The authors conclude the study by saying that further studies into the underlying causes nonendometrioid uterine cancer are needed to fully understand the increase in incidence rates among women in the US.
Journal reference:
Clarke, M., et al. (2019). Hysterectomy-Corrected Uterine Corpus Cancer Incidence Trends and Differences in Relative Survival Reveal Racial Disparities and Rising Rates of Nonendometrioid Cancers. Journal of Clinical Oncology. doi/full/10.1200/JCO.19.00151






















.png)












No hay comentarios:
Publicar un comentario