
Can Oxygen “Microbubbles” Make Radiation Therapy More Effective?
February 20, 2018, by NCI Staff
A new study in mice raises the possibility that microscopic, oxygen-carrying bubbles may help to improve the treatment of breast cancer.In the NCI-supported study, researchers used these “microbubbles” and ultrasound waves to increase the amount of oxygen within tumors. This treatment, they found, greatly improved the ability of radiation therapy to slow breast tumors growing in the mice. The approach also increased how long the mice lived without their disease progressing compared with mice that did not receive the microscopic bubbles prior to radiation treatment.
The new research was published January 21 in the International Journal of Radiation Oncology*Biology*Physics.
If the approach can be translated to humans, “we could potentially get a lot more ‘bang for our buck’ with radiation in terms of treating a tumor, without increasing toxicity,” said the study’s lead investigator, John Eisenbrey, Ph.D., of Thomas Jefferson University.
Supplying Oxygen to Boost Radiation Therapy
Radiation therapy is a mainstay of modern cancer treatment. For example, about half of all women with breast cancer will receive radiation at some point during treatment.
But many tumors are resistant to the cell-killing effects of radiation. Much of this resistance is caused by the low levels of oxygen often found in tumors: oxygen is required for radiation therapy to generate the molecules, called free radicals, that kill cancer cells. When oxygen levels in a tumor are low, radiation therapy is less effective.
For decades, researchers have tested different ways of increasing the amount of oxygen in tumors, said Eric Bernhard, Ph.D., chief of the Radiotherapy Development Branch in NCI’s Division of Cancer Treatment and Diagnosis, who was not involved in the study.
These approaches range from putting patients in hyperbaric chambers before radiation therapy to using drugs that increase blood flow or the number of blood cells that carry oxygen, explained Dr. Eisenbrey.
Unfortunately, because the human body is programmed to keep blood oxygen levels steady, these systemic approaches have largely failed, he added. So his team decided to see if microbubbles—constructs the size of red blood cells that are used for medical imaging—could work in a localized, mechanical way to transport oxygen to tumors.
After manufacturing their microbubbles, the researchers first tested whether the bubbles, when triggered by an ultrasound pulse, could drive oxygen into tumor tissue of mice bearing human breast tumors. To do this, the team first injected the microbubbles into the bloodstream. After the bubbles had circulated throughout the body, ultrasound was aimed at the tumors to “pop” the bubbles and drive oxygen into the tumor tissue.
But many tumors are resistant to the cell-killing effects of radiation. Much of this resistance is caused by the low levels of oxygen often found in tumors: oxygen is required for radiation therapy to generate the molecules, called free radicals, that kill cancer cells. When oxygen levels in a tumor are low, radiation therapy is less effective.
For decades, researchers have tested different ways of increasing the amount of oxygen in tumors, said Eric Bernhard, Ph.D., chief of the Radiotherapy Development Branch in NCI’s Division of Cancer Treatment and Diagnosis, who was not involved in the study.
These approaches range from putting patients in hyperbaric chambers before radiation therapy to using drugs that increase blood flow or the number of blood cells that carry oxygen, explained Dr. Eisenbrey.
Unfortunately, because the human body is programmed to keep blood oxygen levels steady, these systemic approaches have largely failed, he added. So his team decided to see if microbubbles—constructs the size of red blood cells that are used for medical imaging—could work in a localized, mechanical way to transport oxygen to tumors.
After manufacturing their microbubbles, the researchers first tested whether the bubbles, when triggered by an ultrasound pulse, could drive oxygen into tumor tissue of mice bearing human breast tumors. To do this, the team first injected the microbubbles into the bloodstream. After the bubbles had circulated throughout the body, ultrasound was aimed at the tumors to “pop” the bubbles and drive oxygen into the tumor tissue.
Verifying an Oxygen Boost
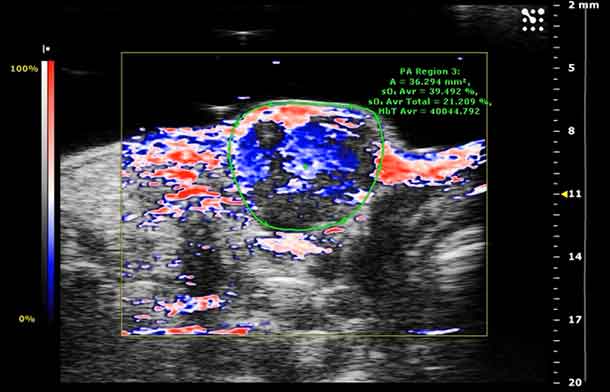
The team then used both a mechanical probe and a type of imaging, called photoacoustic imaging, to measure oxygen in tumors before and after microbubble injection and ultrasound.
Using the probe, they found that on average, after the ultrasound pulse, oxygen in tumors increased to a level that would render cells sensitive to radiation, and these levels were maintained for at least 2 minutes.
Photoacoustic imaging showed that transportation of oxygen in the tumors did not rely on a molecule in the bloodstream called hemoglobin. The researchers were not expecting this, Dr. Eisenbrey said. But, he continued, the lack of dependence on hemoglobin transport may explain how the oxygen molecules also reached parts of the tumor not immediately adjacent to the blood vessels carrying the microbubbles.
“Originally, the hypothesis was that we would only be delivering oxygen where there’s active blood supply,” he said. “But once the oxygen bubbles pop, [the oxygen] actually gets transported out of the blood supply and into the oxygen-depleted parts of the tumor,” he added.
Photoacoustic imaging showed that transportation of oxygen in the tumors did not rely on a molecule in the bloodstream called hemoglobin. The researchers were not expecting this, Dr. Eisenbrey said. But, he continued, the lack of dependence on hemoglobin transport may explain how the oxygen molecules also reached parts of the tumor not immediately adjacent to the blood vessels carrying the microbubbles.
“Originally, the hypothesis was that we would only be delivering oxygen where there’s active blood supply,” he said. “But once the oxygen bubbles pop, [the oxygen] actually gets transported out of the blood supply and into the oxygen-depleted parts of the tumor,” he added.
Approach Improves Outcomes
Next, the researchers tested whether the microbubble treatment made the tumors more sensitive to radiation therapy. For this analysis, they divided similar tumor-bearing mice into five groups.
One control group received radiation alone. A second control group received the oxygen microbubbles and ultrasound but no radiation therapy. The third control group received the oxygen microbubbles and radiation, but no ultrasound triggering. A final control group received nitrogen-containing microbubbles, ultrasound, and radiation therapy. The experimental group received the oxygen microbubbles and ultrasound plus radiation therapy.
The mice in the experimental group that received all three parts of the treatment had the best outcomes. Though the effect of the oxygen microbubbles varied between animals, on average, it delayed tumor growth by about a month and lowered the rate of growth compared with the four other groups. The mice in the experimental group also lived longer without showing any symptoms of progressing cancer.
Interestingly, the mice that received nitrogen microbubbles followed by radiation showed a slight reduction in tumor growth compared with the other two control groups. Previous studies have shown that the mechanical damage caused by microbubbles popping can, on its own, provide some sensitization to radiation, explained Dr. Eisenbrey.
The mice in the experimental group that received all three parts of the treatment had the best outcomes. Though the effect of the oxygen microbubbles varied between animals, on average, it delayed tumor growth by about a month and lowered the rate of growth compared with the four other groups. The mice in the experimental group also lived longer without showing any symptoms of progressing cancer.
Interestingly, the mice that received nitrogen microbubbles followed by radiation showed a slight reduction in tumor growth compared with the other two control groups. Previous studies have shown that the mechanical damage caused by microbubbles popping can, on its own, provide some sensitization to radiation, explained Dr. Eisenbrey.
Moving the Technique into Human Trials
A potential advantage of a microbubble-based approach for improving the response to radiation therapy, said Dr. Eisenbrey, is that many microbubble products have already been approved by the Food and Drug Administration for use in diagnostic imaging. That may make it easier to get approval from the agency to test them as part of cancer therapy in a human trial.
The team has already launched a microbubble trial in people with liver cancer, though this trial is only using the bubbles to cause mechanical damage to cancer cells, not to deliver oxygen.
A few kinks need to be worked out of the oxygen-carrying microbubble approach before it could be tested in people, Dr. Eisenbrey added. These include extending the time oxygen levels are raised in tumor tissue, to match the longer duration needed to deliver radiation therapy in the clinic.
The team would also like to test the system in models of other cancer types, including glioblastoma, liver cancer, and head and neck cancer.
"Combining oxygen-carrying microbubbles with ultrasound-triggered delivery to solid tumors is a novel approach to enhancing tumor oxygenation and sensitivity to radiation, and it deserves further study," concluded Dr. Bernhard.
The team has already launched a microbubble trial in people with liver cancer, though this trial is only using the bubbles to cause mechanical damage to cancer cells, not to deliver oxygen.
A few kinks need to be worked out of the oxygen-carrying microbubble approach before it could be tested in people, Dr. Eisenbrey added. These include extending the time oxygen levels are raised in tumor tissue, to match the longer duration needed to deliver radiation therapy in the clinic.
The team would also like to test the system in models of other cancer types, including glioblastoma, liver cancer, and head and neck cancer.
"Combining oxygen-carrying microbubbles with ultrasound-triggered delivery to solid tumors is a novel approach to enhancing tumor oxygenation and sensitivity to radiation, and it deserves further study," concluded Dr. Bernhard.





















.png)












No hay comentarios:
Publicar un comentario