
FDA Approves New Treatment for Certain Neuroendocrine Tumors
February 8, 2018, by NCI Staff
People with certain cancerous neuroendocrine tumors (NETs) affecting the digestive tract now have a new treatment option.
On January 29, the Food and Drug Administration (FDA) approved a new targeted treatment, lutetium Lu 177 dotatate (Lutathera®), for adult patients with advanced NETs that affect the pancreas or gastrointestinal tract, known as GEP-NETs. Lutetium Lu 177 dotatate is the first radioactive drug approved to treat these rare cancers.
Patients with GEP-NETs have limited treatment options if initial therapy fails to keep the cancer from growing or progressing.
“This is a major advance for patients with neuroendocrine tumors and provides a new treatment alternative for a good number of patients who don’t respond to other treatments,” said Electron Kebebew, M.D., chief of the Endocrine Oncology Branch in NCI's Center for Cancer Research.
The new drug consists of a radioactive isotope, Lu-177, attached to dotatate—a molecule that binds to GEP-NET cells that have a molecule called a somatostatin receptor on their surface. The drug then enters these somatostatin receptor−positive tumor cells, and radiation emitted by Lu-177 helps kill the cells.
New Approval Supported by Two Studies
The FDA approval was based on results from two clinical studies. The first study, was a randomized clinical trial of 229 patients with inoperable, somatostatin receptor−positive NETs in the midgut that had gotten worse after treatment with standard-dose octreotide LAR (Sandostatin® LAR Depot). The multisite trial, called NETTER-1, compared lutetium Lu 177 dotatate plus standard-dose octreotide LAR with high-dose octreotide LAR, and was funded by the drug’s manufacturer, Advanced Accelerator Applications.
Patients in NETTER-1 who were treated with lutetium Lu 177 dotatate lived substantially longer without their cancer progressing than patients who received high-dose octreotide LAR.
In addition, FDA considered findings from a study in the Netherlands of 1,214 patients with somatostatin receptor−positive tumors, including 360 with GEP-NETs. Patients in this single-site study received lutetium Lu 177 dotatate as part of a program that provides access to experimental drugs for patients with serious diseases who lack treatment alternatives. Complete or partial tumor shrinkage was reported in 16% of the patients with GEP-NETs.
Serious side effects of lutetium Lu 177 dotatate in the two studies were rare. They included low levels of blood cells, development of certain blood or bone marrow cancers (secondary myelodysplastic syndrome and leukemia), kidney damage, liver damage, abnormal levels of hormones in the body (neuroendocrine hormonal crises), and infertility.
Diagnostic Imaging Will Help Identify Patients Who Could Benefit from Drug
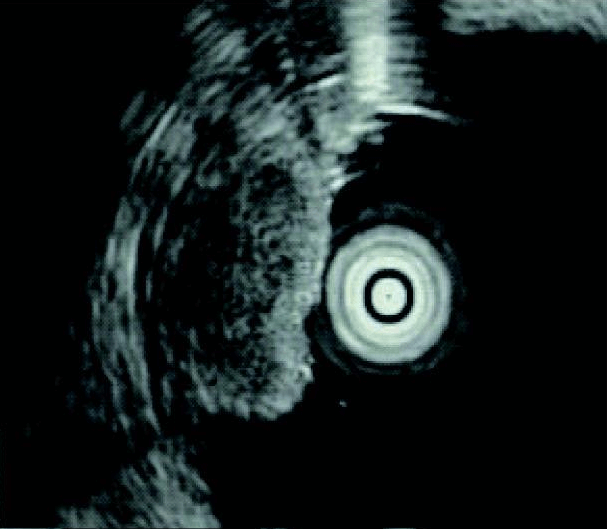
Most GEP-NET patients have tumors that express somatostatin receptors. In June 2016, FDA approved a diagnostic imaging method that uses dotatate tagged with a different radioactive element, gallium-68, to locate somatostatin receptor–positive tumors using positron emission tomography (PET) scans.
“That was a major step forward,” Dr. Kebebew said. “If you do imaging with dotatate, then you can know up front whether the dotatate [in the lutetium Lu 177 dotatate] is likely to be taken up by the tumor” and help kill the tumor cells.
This dotatate-based approach is much more sensitive than older methods used to detect somatostatin receptor–positive GEP-NETs, which means more patients are likely to be identified as candidates for treatment with the new drug, Dr. Kebebew explained.
“As with any new treatment, we will need to better define who is likely to benefit from it,” he continued. Many people with GEP-NETs have disease that doesn’t progress for a long time even without treatment, he said.
In addition, Dr. Kebebew said, “we always need long-term follow-up studies to make sure there are no toxicities [of the drug] that weren’t observed in the initial clinical trials.”





















.png)












No hay comentarios:
Publicar un comentario