Lyme Disease: Gene Signatures May Catch the Infection Sooner
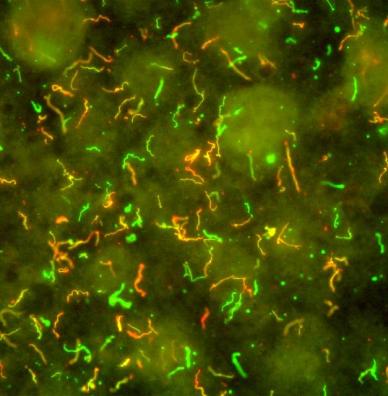
Caption: Borrelia burgdorferi. Immunofluorescent antibodies bind to surface proteins on the bacterium that causes Lyme disease, producing fluorescent yellow, red, and green hues.
Credit: National Institute of Allergy and Infectious Diseases
Credit: National Institute of Allergy and Infectious Diseases
Each year, thousands of Americans are bitten by deer ticks.These tiny ticks, common in and around wooded areas in some parts of the United States, can transmit a bacterium into the bloodstream that causes Lyme disease. Those infected experience fever, headache, stiff necks, body aches, and fatigue. A characteristic circular “target” red rash can mark the site of the tick bite, but isn’t always noticed. In fact, many people don’t realize that they’ve been bitten, and weeks can pass before they see a doctor. By then the infection has spread, sometimes causing additional rashes and/or neurological, cardiac, and rheumatological symptoms that mimic those of other conditions. All of this can make getting the right diagnosis frustrating, especially in areas where Lyme disease is rare.
Even when Lyme disease is suspected early on, the bacterium is unusually slow growing and present at low levels, so it can take a while before blood tests detect antibodies to confirm the condition. By then, knocking out the infection with antibiotics can be more challenging. But research progress continues to be made toward improving the diagnosis of Lyme disease.
An NIH-supported team recently uncovered a unique gene expression pattern in white blood cells from people infected with the Lyme disease-causing bacterium Borrelia burgdorferi [1]. This distinctive early gene signature, which persists after antibiotic treatment, is unique from other viral and bacterial illnesses studies by the team. With further work and validation, the test could one day possibly provide a valuable new tool to help doctors diagnose Lyme disease earlier and help more people get the timely treatment that they need.
The new study, published in the online journal mBio, was led by researchers Charles Chiu of the University of California, San Francisco, and John Aucott of Johns Hopkins University, Baltimore. The Hopkins group enrolled 29 adults from Maryland with newly diagnosed Lyme disease and 13 healthy adult controls. For the Lyme patients, blood samples were taken at three time points: 1) immediately upon their diagnosis, 2) just after they’d completed a standard, 3-week course with antibiotic doxycycline taken orally, and 3) 6 months after treatment.
By the end of the study, about half of the patients had made a full recovery. The others continued to contend with lingering fatigue, joint pain, cognitive dysfunction, and other symptoms. Four people later were diagnosed with post-treatment Lyme disease syndrome (PTLDS) based on a documented functional decline over time. It’s estimated that, for still unknown reasons, 10 to 20 percent of people with Lyme disease progress to PTLDS. That doesn’t appear to represent ongoing infection, but some disruption of the immune system that persists after the pathogen has been eliminated.
Hoping to get a better handle on these varied treatment outcomes, the researchers turned their attention to various types of immune cells in the patient blood samples. Because the immune system typically responds differently to different infections, the researchers wondered whether these white blood cells produce a distinctive gene signature when mounting a response to B. burgdorferi. To get the answer, they compared the transcriptomes—the RNA gene transcripts expressed by a cell’s genome at a given time—of people with Lyme disease to those from the healthy controls.
Their analyses uncovered changes in the expression of more than 1,000 genes at the time of diagnosis. Many of the changes reflect inflammatory and immune responses, as expected in a person battling an infection. Further analyses showed that just under half of the observed differences in gene expression were shared with other common illnesses, making Lyme disease a relatively unique infection. Interestingly, the gene expression signature in early Lyme disease had more in common with viral influenza infections than infections caused by other bacteria.
For the vast majority of infectious diseases, effective treatment allows the immune system to stop fighting and return gene expression levels to normal. Remarkably, that was not the case with Lyme disease. The immune cells had post-treatment transcriptomes that varied from those of healthy controls by about 1,000 genes. This signature also included many of the underlying inflammatory and immune features seen in the pre-treatment response, and even as patients began to feel better.
While more research is required, this unusual finding suggests there’s hope for developing more effective diagnostic tests for Lyme disease. Chiu’s team is already working to learn more about the Lyme signature and is attempting to devise a panel of 50 to 100 genes that may be specific to the acute, early phase of the infection.
With only four people in the study receiving a diagnosis of PTLDS, the researchers didn’t find many clues to explain why treatment helps some people bounce back quickly while others don’t. For that, larger studies will be needed. But the findings already have revealed multiple genes and gene pathways that had not been associated with Lyme disease previously, and may point the way to new approaches to therapy. In fact, the signature 6 months after treatment showed intriguing similarities with autoimmune diseases, including lupus, rheumatoid arthritis, and chronic fatigue syndrome.
Every year, health departments around the country report a total of about 30,000 confirmed cases of Lyme disease [2]. That makes Lyme disease the leading vector-borne illness in the United States. But many cases are never diagnosed, and the true incidence is likely at least 10-fold higher. These new findings add to other recent research that looks beyond traditional diagnostics to identify disease-causing biomarkers for Lyme disease [3] and suggest possible avenues for improving its diagnosis and treatment.
References:
[1] Longitudinal Transcriptome Analysis Reveals a Sustained Differential Gene Expression Signature in Patients Treated for Acute Lyme. Bouquet J, Soloski MJ, Swei A, Cheadle C, Federman S, Billaud JN, Rebman AW, Kabre B, Halpert R, Boorgula M, Aucott JN, Chiu CY. mBio. 2016 Feb 12;7(1): e00100-16.
[2] How many people get Lyme Disease? Centers for Disease Control and Prevention. 2015 Sept 30.
[3] Development of a metabolic biosignature for detection of early Lyme disease. Mollins CR, Ashton LV, Wormser GP, Hess AM, Delorey MJ, Mahapatra S, Schriefer ME, Belisle JT. Clin Infect Dis. 2015 Jun 15;60(12):1767-1775.
Links:
Lyme Disease (National Institute of Allergy and Infectious Diseases/NIH)
Lyme Disease Maps (Centers for Disease Control and Prevention)
“Genome reveals insights into tick that spreads Lyme disease,” NIH Research Matters, February 23, 2016.
Research at the Lyme Center (Johns Hopkins University, Baltimore)
Charles Chiu (University of California, San Francisco)
NIH Support: National Heart, Lung, and Blood Institute; National Institute of Arthritis and Musculoskeletal and Skin Diseases





















.png)












No hay comentarios:
Publicar un comentario