HIV Among People Aged 50 and Older
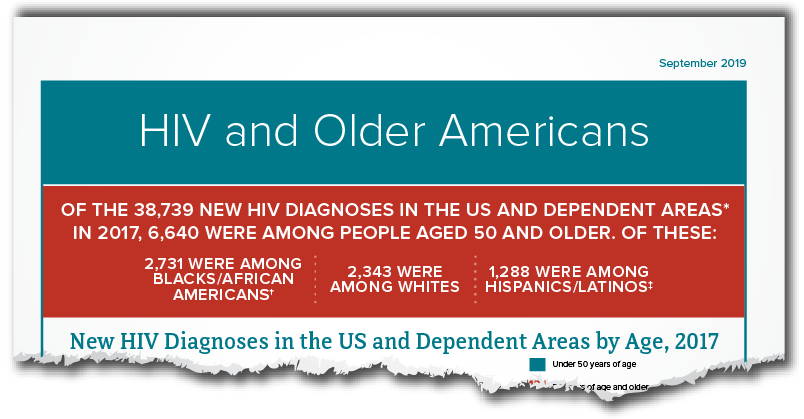
Nearly half of people in the United States living with diagnosed HIV are aged 50 and older. Though new HIV diagnoses are declining among people aged 50 and older, around 1 in 6 HIV diagnoses in 2016 were in this group.
The Numbers
HIV Diagnosesa
- People aged 50 and older accounted for 17% (6,812) of the 39,782 new HIV diagnoses in 2016 in the United States. People aged 50 to 54 accounted for 43% (2,959) of the new diagnoses among people aged 50 and older.b
- Among people aged 50 and older, blacks/African Americans accounted for 42% of all new HIV diagnoses in 2016. Whites accounted for 37%, Hispanics/Latinosc accounted for 18%, and other races/ethnicities accounted for 4%.
- Among people aged 50 and older, 49% of new HIV diagnoses in 2016 were among gay and bisexual men,d 15% were among heterosexual men, 24% were among heterosexual women, and 12% were among people who inject drugs.e
- From 2011 to 2015, HIV diagnoses among all people aged 50 and older decreased by 7%.
- In 2016, 35% of people aged 50 and older already had late stage infection (AIDS) when they received an HIV diagnosis (i.e., they received a diagnosis late in the course of the infection). But that percentage has declined since 2011, when 42% already had late stage infection.
HIV Diagnoses by Age, 2016, United States
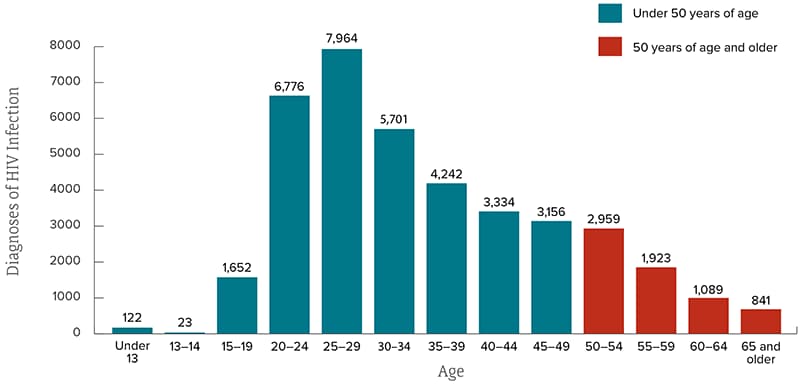
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2016. HIV Surveillance Report 2016;28.
Living With HIV and Deaths
- In 2015, an estimated 47% (454,684) of Americans with diagnosed HIV were aged 50 and older. Of these, 38% (171,172) were aged 50-54, 29% (131,430) were aged 55-59, 18% (81,438) were aged 60-64, and 16% (70,644) were aged 65 and older.
- Among all people aged 55 and older with HIV in 2015, 95% had received a diagnosis, 69% received HIV medical care, 56% received continuous HIV care, and 60% had a suppressed viral load.f By comparison, 86% of all people with HIV had received a diagnosis, and 51% had a suppressed viral load at the time of their last test. A person with HIV who takes HIV medicine as prescribed and gets and stays virally suppressed can stay healthy and has effectively no risk of sexually transmitting HIV to HIV-negative partners.
- In 2015, 2,749 people aged 55 and older died from HIV disease.
People Living With Diagnosed HIV by Age, 2015, United States
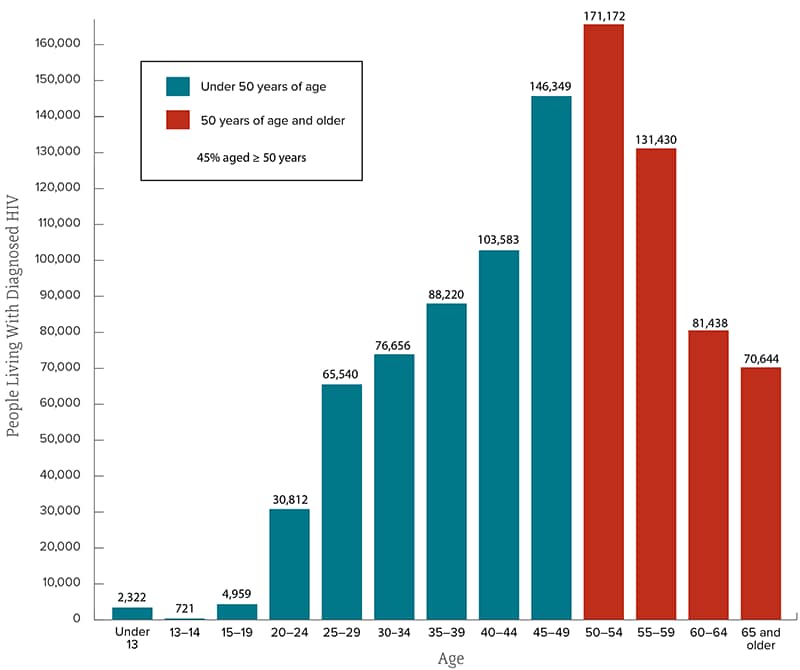
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2016. HIV Surveillance Report 2016;28.
Prevention Challenges
Older people in the United States are more likely than younger people to have late-stage HIV infection at the time of diagnosis, which means they start treatment late and possibly suffer more immune-system damage. Late diagnoses can occur because health care providers may not always test older people for HIV infection. Also, older people may not consider themselves to be at risk of HIV infection or may mistake HIV symptoms for those of normal aging and not consider HIV as a cause. Among people aged 55 and older who received an HIV diagnosis in 2015, 50% had HIV 4.5 years before diagnosis—the longest diagnosis delay for any age group.
Older people may have many of the same HIV risk factors as younger people, including a lack of knowledge about HIV prevention and sexual risk including having multiple sex partners. Older people also face some unique issues:
- Women who no longer worry about becoming pregnant may be less likely to use a condom and to practice safer sex. Age-related thinning and dryness of vaginal tissue may raise older women’s risk for HIV infection.
- Although they visit their doctors more frequently, older people are less likely than younger people to discuss their sexual or drug use behaviors with their doctors. And doctors are less likely to ask their older patients about these issues.
Stigma is a particular concern among older people because they may already face isolation due to illness or loss of family and friends. Stigma negatively affects people’s quality of life, self-image, and behaviors, and may prevent them from seeking HIV care and disclosing their HIV status.
Aging with HIV infection also presents special challenges for preventing other diseases because both age and HIV increase risk for cardiovascular disease, bone loss, and certain cancers. Older HIV patients and their care providers need to maximize prevention efforts against these conditions and remain vigilant for early signs of illness. They also need to be careful about interactions between the medications used to treat HIV and those used to treat common age-related conditions such as hypertension, diabetes, elevated cholesterol, and obesity.
What CDC Is Doing
CDC and its partners are working together to maximize the effectiveness of current HIV prevention methods and improve surveillance among all people in the United States. For example,
- Support for health departments and community-based organizations to deliver effective prevention interventions. A new funding opportunitydirects resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the United States.
- CDC provides support and technical assistance to health departments and community-based organizations to deliver effective prevention and evidence-based interventions for antiretroviral therapy adherence for older Americans.
- CDC is awarding approximately $130 million over 5 years (2014-2019) to provide training and technical assistance for staff of health departments, community-based organizations, and health care organizations to help them link people with HIV to care, retain or re-engage them in care, and help them achieve viral suppression.
- Act Against AIDS, a national communications initiative, focuses on raising awareness, fighting stigma, and reducing the risk of HIV infection among at-risk populations. Act Against AIDS includes
- Let’s Stop HIV Together, which raises awareness that we all have a role to play in stopping HIV stigma.
- Doing It, which motivates individuals to get tested for HIV and know their status.
- Start Talking. Stop HIV., which encourages open discussion among gay and bisexual men about a range of HIV prevention strategies and related sexual health issues.
- HIV Treatment Works., which helps people with HIV stay healthy, protect others, and live longer, healthier lives.
- Partnering and Communicating Together (PACT), a 5-year partnership with organizations such as the National Hispanic Medical Association to raise awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV.
For additional information and resources, visit:
- Administration on Aging
- POZ
- Services & Advocacy for LGBT Elders
- HIV and Older Adults
- The Well Project
a HIV diagnoses indicate when a person was diagnosed with HIV, not when the person was infected.
b Data for 2016 are preliminary (subject to change) because they are based on only a 6-month reporting delay. Data for 2016 should not be used when assessing trends.
c Hispanics/Latinos can be of any race.
d The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
e People who inject drugs includes infections attributed to injection drug use and other sexual risk factors.
f Viral suppression is defined as having fewer than 200 copies of the virus per milliliter of blood on the most recent viral load test in 2015. Receiving continuous HIV care is defined as having two viral load or CD4 tests 3 or more months apart in 2015. (CD4 cells are the cells in the body’s immune system that are destroyed by HIV.)
b Data for 2016 are preliminary (subject to change) because they are based on only a 6-month reporting delay. Data for 2016 should not be used when assessing trends.
c Hispanics/Latinos can be of any race.
d The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
e People who inject drugs includes infections attributed to injection drug use and other sexual risk factors.
f Viral suppression is defined as having fewer than 200 copies of the virus per milliliter of blood on the most recent viral load test in 2015. Receiving continuous HIV care is defined as having two viral load or CD4 tests 3 or more months apart in 2015. (CD4 cells are the cells in the body’s immune system that are destroyed by HIV.)





















.png)












No hay comentarios:
Publicar un comentario