Meat and Poultry Processing Workers and Employers
Interim Guidance from CDC and the Occupational Safety and Health Administration (OSHA)
Meat and poultry processing facilities are a component of the critical infrastructure within the Food and Agriculture Sector. CDC’s Critical Infrastructure Guidance advises that critical infrastructure workers may be permitted to continue work following potential exposure to COVID-19, provided they remain asymptomatic and additional precautions are implemented to protect them and the community. All meat and poultry processing facilities developing plans for continuing operations in the setting of COVID-19 occurring among workers or in the surrounding community should (1) work directly with appropriate state and local public health officials and occupational safety and health professionals; (2) incorporate relevant aspects of CDC guidance, including but not limited to this document and the CDC’s Critical Infrastructure Guidance; and (3) incorporate guidance from other authoritative sources or regulatory bodies as needed.
Multiple outbreaks of COVID-19 among meat and poultry processing facility workers have occurred in the United States recently. This document provides guidance for meat and poultry processing workers and employers—including those involved in beef, pork, and poultry operations. This guidance supplements but does not replace general guidance at these web sites:
- osha.gov/coronavirus
- https://www.cdc.gov/coronavirus/2019-ncov/index.html
- https://www.cdc.gov/coronavirus/2019-ncov/community/critical-workers/implementing-safety-practices.html
Coronavirus disease 2019 (COVID-19) is a respiratory illness caused by a new virus called SARS-CoV-2. Symptoms often include a fever, cough, and shortness of breath and can range from very mild to severe. Some people become so sick they must be admitted to the hospital, and some people may die from the illness. Our understanding about the new virus and how the virus spreads is evolving as we learn more about COVID-19, so check the CDC website for the latest information. The virus is thought to spread mainly from person to person:
- Between people who are in close contact with one another (within about six feet, which is about two meters).
- Through respiratory droplets produced when an infected person coughs, sneezes, or talks.
Recent studies indicate that people who are not showing symptoms can spread the virus. It may also be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes. This is not thought to be the main way the virus spreads, but we are still learning more about this virus. Workers at higher risk for serious illness include older adults and people of any age with chronic medical conditions. Policies and procedures addressing issues related to workers at higher risk of serious illness should be made in consultation with occupational medicine and human resource professionals.
Exposure risk among meat and poultry processing workers
Workers involved in meat and poultry processing are not exposed to SARS-CoV-2 through the meat products they handle. However, their work environments—processing lines and other areas in busy plants where they have close contact with coworkers and supervisors—may contribute substantially to their potential exposures. The risk of occupational transmission of SARS-CoV-2 depends on several factors. Some of these factors are described in the U.S. Department of Labor and U.S. Department of and Health and Human Services’ booklet Guidance on Preparing Workplaces for COVID-19. Distinctive factors that affect workers’ risk for exposure to SARS-CoV-2 in meat and poultry processing workplaces include:
- Distance between workers – meat and poultry processing workers often work close to one another on processing lines. Workers may also be near one another at other times, such as when clocking in or out, during breaks, or in locker/changing rooms.
- Duration of contact – meat and poultry processing workers often have prolonged closeness to coworkers (e.g., for 10-12 hours per shift). Continued contact with potentially infectious individuals increases the risk of SARS-CoV-2 transmission.
- Type of contact – meat and poultry processing workers may be exposed to the infectious virus through respiratory droplets in the air – for example, when workers in the plant who have the virus cough or sneeze. It is also possible that exposure could occur from contact with contaminated surfaces or objects, such as tools, workstations, or break room tables. Shared spaces such as break rooms, locker rooms, and entrances/exits to the facility may contribute to their risk.
- Other distinctive factors that may increase risk among these workers include:
- A common practice at some workplaces of sharing transportation such as ride-share vans or shuttle vehicles, car-pools, and public transportation
- Frequent contact with fellow workers in community settings in areas where there is ongoing community transmission.
Create a COVID-19 assessment and control plan
A qualified workplace coordinator should be identified who will be responsible for COVID-19 assessment and control planning. All workers in the facility should know how to contact the identified coordinator with any COVID-19 concerns. Infection control and occupational safety and health plans should apply to anyone entering or working in the plant (e.g., all facility workers, contractors, and others). Facility management should reach out to state and/or local public health officials and occupational safety and health professionals and establish ongoing communications to make sure they are getting relevant and up-to-date information concerning COVID-19. The workplace coordinators and management should also be aware of and follow all applicable federal regulations and public health agency guidelines. Worksite assessments to identify COVID-19 risks and prevention strategies should be done periodically as part of sound occupational health and public health practice. As part of these assessments, facilities should consider the appropriate role for testing and workplace contact tracing (identifying person-to-person spread) of COVID-19-positive workers in a worksite risk assessment, following available CDC guidance.
Controls
Worker infection prevention recommendations are based on an approach known as the hierarchy of controls. This approach groups actions by their effectiveness in reducing or removing hazards. In most cases, the preferred approach is to eliminate a hazard or processes; install engineering controls; and implement appropriate cleaning, sanitation, and disinfection practices to reduce exposure or shield workers. Administrative controls are also an important part of an approach to prevention in these workplaces.
Engineering Controls
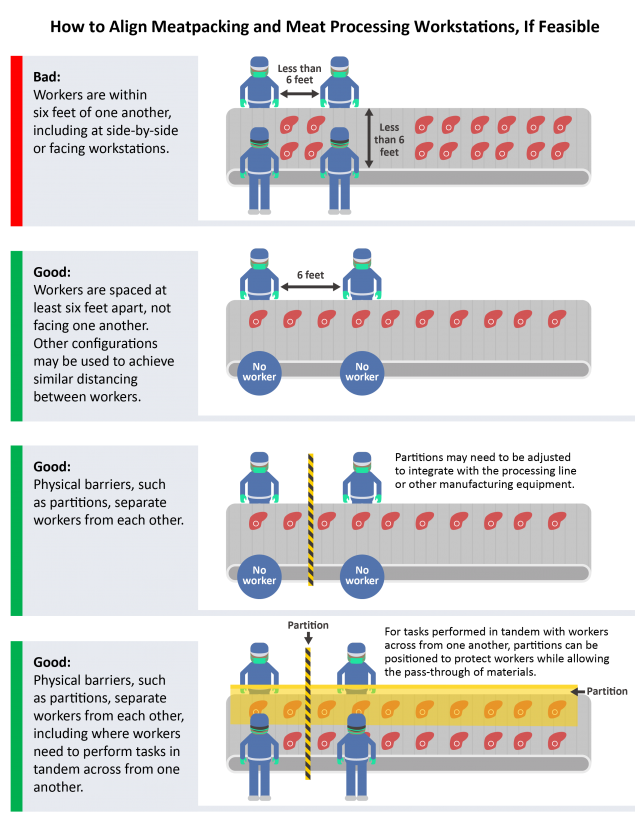
Configure communal work environments so that workers are spaced at least six feet apart, if possible. Current information about the asymptomatic spread of SARS-CoV-2 supports the need for social distancing and other protective measures within a meat and poultry processing work environment. Changes in production practices may be necessary in order to maintain appropriate distances among workers.
Modify the alignment of workstations, including along processing lines, if feasible, so that workers are at least six feet apart in all directions (e.g., side-to-side and when facing one another), when possible. Ideally, modify the alignment of workstations so that workers do not face one another. Consider using markings and signs to remind workers to maintain their location at their station away from each other and practice social distancing on breaks.
Use physical barriers, such as strip curtains, plexiglass or similar materials, or other impermeable dividers or partitions, to separate meat and poultry processing workers from each other, if feasible.
Facilities should consider consulting with a heating, ventilation, and air conditioning engineer to ensure adequate ventilation in work areas to help minimize workers’ potential exposures.
If fans such as pedestal fans or hard mounted fans are used in the facility, take steps to minimize air from fans blowing from one worker directly at another worker. Personal cooling fans should be removed from the workplace to reduce the potential spread of any airborne or aerosolized viruses. If fans are removed, employers should remain aware of, and take steps to prevent, heat hazards.
Place handwashing stations or hand sanitizers with at least 60% alcohol in multiple locations to encourage hand hygiene. If possible, choose hand sanitizer stations that are touch-free. See OSHA’s Sanitation Standard (29 CFR 1910.141), which requires employers to provide handwashing facilities for workers.
Add additional clock in/out stations, if possible, that are spaced apart, to reduce crowding in these areas. Consider alternatives such as touch-free methods or staggering times for workers to clock in/out.
Remove or rearrange chairs and tables, or add partitions to tables, in break rooms and other areas workers may frequent to increase worker separation. Identify alternative areas to accommodate overflow volume such as training and conference rooms, or using outside tents for break and lunch areas.
Administrative Controls
Employers should do the following to promote social distancing:
- Encourage single-file movement with a six-foot distance between each worker through the facility, where possible.
- Designate workers to monitor and facilitate distancing on processing floor lines.
- Stagger break times or provide temporary break areas and restrooms to avoid groups of workers during breaks. Workers should maintain at least six feet of distance from others at all times, including on breaks.
- Stagger workers’ arrival and departure times to avoid congregations of workers in parking areas, locker rooms, and near time clocks.
- Provide visual cues (e.g., floor markings, signs) as a reminder to workers to maintain social distancing.
- Encourage workers to avoid carpooling to and from work, if possible
- If carpooling or using company shuttle vehicles is a necessity for workers, the following control practices should be used:
- Limit the number of people per vehicle as much as possible. This may mean using more vehicles.
- Encourage employees to maintain social distancing as much as possible.
- Encourage employees to use hand hygiene before entering the vehicle and when arriving at the destination.
- Encourage employees in a shared van or car space to wear cloth masks.
- Clean and disinfect commonly touched surfaces after each carpool or shuttle trip (e.g., door handles, handrails, seatbelt buckles).
- Encourage employees to follow coughing and sneezing etiquette when in the vehicle.
- If carpooling or using company shuttle vehicles is a necessity for workers, the following control practices should be used:
Employers may determine that modifying processing or production lines, shifts, and staggering workers across shifts would help to maintain overall meat and poultry processing capacity while measures to minimize exposure to SARS-CoV-2 are in place. For example, a plant that normally operates on one daytime shift may be able to split workers into two or three shifts throughout a 24-hour period. In meat and poultry processing plants, one shift may need to be reserved for cleaning and sanitization.
Monitor and respond to absenteeism at the workplace. Implement plans to continue essential business functions in cases of higher than usual absenteeism.
Review leave and incentivize policies:
- Analyze sick leave policies and consider modifying them to make sure that ill workers are not in the workplace. Make sure that employees are aware of and understand these policies.
- Analyze any incentive programs and consider modifying them, if warranted, so that employees are not penalized for taking sick leave if they have COVID-19.
- Additional flexibilities might include giving advances on future sick leave and allowing employees to donate sick leave to each other.
Consider cohorting (grouping together) workers. This can increase the effectiveness of altering the plant’s normal shift schedules by making sure that groups of workers are always assigned to the same shifts with the same coworkers. Cohorting may reduce the spread of workplace SARS-CoV-2 transmission by minimizing the number of different individuals who come into close contact with each other over the course of a week. Cohorting may also reduce the number of workers quarantined because of exposure to the virus.
Establish a system for employees to alert their supervisors if they are experiencing signs or symptoms of COVID-19 or if they have had recent close contact with a suspected or confirmed COVID-19 case.
Provide workers access to soap, clean running water, and single use paper towels for handwashing.
- Provide alcohol-based hand sanitizers containing at least 60% alcohol if soap and water are not immediately available.
- Place hand sanitizers in multiple locations to encourage hand hygiene. If possible, choose hand sanitizer stations that are touch-free.
- Consider other workplace programs to promote personal hygiene, such as:
- building additional short breaks into staff schedules to increase how often staff can wash their hands with soap and water or use hand sanitizers with at least 60% alcohol;
- providing tissues and no-touch trash receptacles for workers to use; and
- educating workers that cigarettes and smokeless tobacco use can lead to increased contact between potentially contaminated hands and their mouth, and that avoiding these products may reduce their risk of infection.
Workers should be educated to avoid touching their faces, including their eyes, noses, and mouths, particularly until after they have thoroughly washed their hands upon completing work and/or removing personal protective equipment (PPE).
Cloth face coverings in meat and poultry processing facilities
CDC recommends wearing cloth face coverings as a protective measure in addition to social distancing (i.e., staying at least 6 feet away from others). Cloth face coverings may be especially important when social distancing is not possible or feasible based on working conditions. A cloth face covering may reduce the amount of large respiratory droplets that a person spreads when talking, sneezing, or coughing. Cloth face coverings may prevent people who do not know they have the virus that causes COVID-19 from spreading it to others. Cloth face coverings are intended to protect other people—not the wearer.
Cloth face coverings are not PPE. They are not appropriate substitutes for PPE such as respirators (like N95 respirators) or medical facemasks (like surgical masks) in workplaces where respirators or facemasks are recommended or required to protect the wearer.
While wearing cloth face coverings is a public health measure intended to reduce the spread of COVID-19 in communities, it may not be practical for workers to wear a single cloth face covering for the full duration of a work shift (e.g., eight or more hours) in a meat or poultry processing facility if they become wet, soiled, or otherwise visibly contaminated during the work shift. If cloth face coverings are worn in these facilities, employers should provide readily available clean cloth face coverings (or disposable facemask options) for workers to use when the coverings become wet, soiled, or otherwise visibly contaminated.
Employers who determine that cloth face coverings should be worn in the workplace, including to comply with state or local requirements for their use, should ensure the cloth face coverings:
- fit over the nose and mouth and fit snugly but comfortably against the side of the face;
- are secured with ties or ear loops;
- include multiple layers of fabric;
- allow for breathing without restriction;
- can be laundered using the warmest appropriate water setting and machine dried daily after the shift, without damage or change to shape (a clean cloth face covering should be used each day);
- are not used if they become wet or contaminated;
- are replaced with clean replacements, provided by employer, as needed.
- are handled as little as possible to prevent transferring infectious materials to the cloth; and
- are not worn with or instead of respiratory protection when respirators are needed.
Educate and train workers and supervisors about how they can reduce the spread of COVID-19.
Supplement workers’ normal and required job training (e.g., training required under OSHA standards) with additional training and information about COVID-19, recognizing signs and symptoms of infection, and ways to prevent exposure to the virus. Training should include information about how to implement the various infection prevention and control measures recommended here and included in any infection prevention and control or COVID-19 response plan that an employer develops. OSHA provides additional information about training on its COVID-19 webpage.
All communication and training should be easy to understand and should (1) be provided in languages appropriate to the preferred languages spoken or read by the workers, if possible; (2) be at the appropriate literacy level; and (3) include accurate and timely information about:
- signs and symptoms of COVID-19, how it spreads, risks for workplace exposures, and how workers can protect themselves; and
- proper handwashing practices and use of hand sanitizer stations;
- cough and sneeze etiquette;
- other routine infection control precautions (e.g., signs and symptoms of COVID-19, putting on or taking off masks or cloth face coverings and social distancing measures).
Employers should place simple posters in all of the languages that are common in the worker population that encourage staying home when sick, cough and sneeze etiquette, and proper hand hygiene practices. They should place these posters at the entrance to the workplace and in break areas, locker rooms, and other workplace areas where they are likely to be seen.
- CDC has free, simple posters available to download and print, some of which are translated into different languages. The Stop the Spread of Germs poster is available in Amharic, Arabic, Burmese, Dari, Farsi, French, Haitian Creole, Kinyarwanda, Karen, Korean, Nepali, Pashto, Portuguese, Russian, Simplified Chinese, Somali, Spanish, Swahili, Tigryna, Ukrainian, and Vietnamese.
Employers should post signs that you can read from a far distance (or use portable, electronic reader boards) that inform visitors and workers of social distancing practices.
OSHA understands that some employers may face difficulties complying with OSHA standards due to the ongoing health emergency, including those standards that require certain types of worker training. OSHA is providing enforcement discretion around completion of training and other provisions in its various standards. OSHA has instructed its Compliance Safety and Health Officers (CSHOs) to evaluate whether an employer has made a good faith effort to comply with applicable OSHA standards and, in situations where compliance was not possible given the ongoing pandemic, to ensure that employees were not exposed to hazards from tasks, processes, or equipment for which they were not prepared or trained.
Cleaning and disinfection in meat and poultry processing
For tool-intensive operations, employers should ensure tools are regularly cleaned and disinfected, including at least as often as workers change workstations or move to a new set of tools. Refer to List N on the EPA website for EPA-registered disinfectants that have qualified under EPA’s emerging viral pathogens program for use against SARS-CoV-2.
Establish protocols and provide supplies to increase the frequency of sanitization in work and common spaces. Disinfect frequently touched surfaces in workspaces and break rooms (e.g., microwave or refrigerator handles or vending machine touchpads) at least once per shift, if possible. For example, wipe down tools or other equipment at least as often as workers change workstations. Frequently clean push bars and handles on any doors that do not open automatically and handrails on stairs or along walkways. If physical barriers are being used, then these should be cleaned frequently.
Workers who perform cleaning and disinfection tasks may require additional PPE and other controls to protect them from chemical hazards posed by disinfectants. Note: Employers must ensure their written hazard communication program is up to date and training is up to date for all employees. (Also see OSHA’s enforcement discretion memorandum on this topic.) Employers may need to adapt guidance from this section, the Environmental Services Workers and Employers section, and the Interim Guidance for Workers and Employers of Workers at Increased Risk of Occupational Exposure, to fully protect workers performing cleaning and disinfection activities in manufacturing workplaces.
Screening1 and monitoring workers
Workplaces, particularly in areas where community transmission of COVID-19 is occurring, should consider developing and implementing a comprehensive screening and monitoring strategy aimed at preventing the introduction of COVID-19 into the worksite. Consider a program of screening workers before entry into the workplace, criteria for return to work of exposed and recovered (those who have had signs or symptoms of COVID-19 but have gotten better), and criteria for exclusion of sick workers. This type of program should be coordinated to the extent possible with local public health authorities and could consist of the following activities:
Screening of workers for COVID-19
Screening meat and poultry processing workers for COVID-19 symptoms (such as temperature checks) is an optional strategy that employers may use. If implemented for all workers, policies and procedures for screening workers should be developed in consultation with state and local health officials and occupational medicine professionals. Options to screen workers for COVID-19 symptoms include:
- Screen prior to entry into the facility.
- Provide verbal screening in appropriate language(s) to determine whether workers have had a fever, felt feverish, or had chills, coughing, or difficulty breathing in the past 24 hours.
- Check temperatures of workers at the start of each shift to identify anyone with a fever of 100.4℉ or greater (or reported feelings of feverishness). Ensure that screeners:
- are trained to use temperature monitors and monitors are accurate under conditions of use (such as cold temperatures); and
- wear appropriate PPE.
- Do not let employees enter the workplace if they have a fever of 100.4℉ or greater (or reported feelings of feverishness), or if screening results indicate that the worker is suspected of having COVID-19.
- Encourage workers to self-isolate and contact a healthcare provider;
- Provide information on the facility’s return-to-work policies and procedures; and
- Inform human resources, employer health unit (if in place), and supervisor (so worker can be moved off schedule during illness and a replacement can be assigned, if needed).
Ensure that personnel performing screening activities, including temperature checks, are appropriately protected from exposure to potentially infectious workers entering the facility:
- Implement engineering controls, such as physical barriers or dividers or rope and stanchion systems, to maintain at least six feet of distance between screeners and workers being screened.
- If screeners need to be within six feet of workers, provide them with appropriate PPE based on the repeated close contact the screeners have with other workers.
- Such PPE may include gloves, a gown, a face shield, and, at a minimum, a face mask.
- N95 filtering facepiece respirators (or more protective) may be appropriate for workers performing screening duties and necessary for workers managing a sick employee in the work environment (see below) if that employee has signs or symptoms of COVID-19. If respirators are needed, they must be used in the context of a comprehensive respiratory protection program that includes medical exams, fit testing, and training in accordance with OSHA’s Respiratory Protection standard (29 CFR 1910.134).
Managing sick workers
Workers who appear to have symptoms (e.g., fever, cough, or shortness of breath) upon arrival at work or who become sick during the day should immediately be separated from others at the workplace and sent home.
Ensure that personnel managing sick employees are appropriately protected from exposure. When personnel need to be within six feet of a sick colleague, appropriate PPE may include gloves, a gown, a face shield and, at a minimum, a face mask. N95 filtering facepiece respirators (or more protective) may be appropriate for workers managing a sick employee if that employee has signs or symptoms of COVID-19. If respirators are needed, they must be used in the context of a comprehensive respiratory protection program that includes medical exams, fit testing, and training in accordance with OSHA’s Respiratory Protection standard (29 CFR 1910.134).
If a worker is confirmed to have COVID-19, employers should inform anyone they have come into contact with (including fellow workers, inspectors, graders, etc.) of their possible exposure to COVID-19 in the workplace, but should maintain confidentiality as required by the Americans with Disabilities Act (ADA). The employer should instruct fellow workers about how to proceed based on the CDC Public Health Recommendations for Community-Related Exposure.
If a worker becomes or reports being sick, disinfect the workstation used and any tools handled by the symptomatic worker.
Employers should work with state, local, tribal, and/or territorial health officials to facilitate the identification of other exposed and potentially exposed individuals, such as coworkers in a plant.
On-site healthcare personnel, such as facility nurses or emergency medical technicians, should follow appropriate CDC and OSHA guidance for healthcare and emergency response personnel.
Addressing return to work
- Critical infrastructure employers have an obligation to manage the continuation of work and return to work of their workers in ways that best protect the health of workers, their coworkers, and the general public. Employers should consider providing screening and ongoing medical monitoring of these workers, ensuring they wear an appropriate source control device in accordance with CDC and OSHA guidance, and implementing social distancing to minimize the chances of workers exposing one another.
- Critical infrastructure employers should continue to minimize the number of workers present at worksites, balancing the need to protect workers with support for continuing critical operations.
- Reintegration (bringing back) of exposed, asymptomatic workers to onsite operations should follow the CDC Critical Infrastructure Guidance. The guidance advises that employers may permit workers who have been exposed to COVID-19, but remain without symptoms, to continue to work, provided they adhere to additional safety precautions. Consultation with an occupational health provider and state and local health officials will help employers develop the most appropriate plan consistent with CDC guidance.
- Reintegration of workers with COVID-19 (COVID-19 positive), including those workers who have remained asymptomatic, to onsite operations should follow the CDC interim guidance, “Discontinuation of Isolation for Persons with COVID-19 Not in Healthcare Settings.”
As employers move forward with continuing essential work, they should implement strategies to prioritize positions without which critical work would stop. This prioritization should include an analysis of work tasks, workforce availability at specific worksites, and assessment of hazards associated with the tasks and worksite. Employers may be able to cross-train workers to perform critical duties at a worksite to minimize the total number of workers needed to continue operations.
For workers who have had signs/symptoms of COVID-19
Workers with COVID-19 who have symptoms and have stayed home (home isolated) should not return to work until they have met the criteria to discontinue home isolation, and have consulted with their healthcare providers and state and local health departments.
The situation is constantly changing, so employers of critical infrastructure workers will need to continue to reassess the virus’s transmission levels in their area.
Personal protective equipment
Employers must conduct a hazard assessment to determine if hazards are present, or are likely to be present, for which workers need PPE. OSHA’s PPE standards (29 CFR 1910 Subpart I) require employers to select and provide appropriate PPE to protect workers from hazards identified in the hazard assessment. The results of that assessment will be the basis of workplace controls (including PPE) needed to protect workers.
Employers should:
- Use videos or in-person visual demonstrations of proper PPE donning and doffing procedures. (Maintain social distancing during these demonstrations.)
- Emphasize that care must be taken when putting on and taking off PPE to ensure that the worker or the item does not become contaminated.
- Provide PPE that is either disposable (preferred) or, if reusable, ensure it is properly disinfected and stored in a clean location when not in use.
- PPE worn at the facility should not be taken home or shared.
Face shields may serve as both PPE and source control:
- If helmets are being used, use face shields designed to attach to helmets.
- Face shields can provide additional protection from both potential process-related splashes and potential person-to-person droplet spread.
- Safety glasses may fog up when used in combination with masks or cloth face coverings.
- Only some face shields are acceptable substitutions for eye protection (such as safety glasses) that are used for impact protection; facilities should consult with an occupational safety and health professional concerning the use of face shields.
- Face shields can help minimize contamination of masks and cloth face coverings
- If used, face shields should be cleaned and decontaminated after each shift, and when not in use they should be kept in a clean location at the work facility.
- If used, face shields should also wrap around the sides of the wearer’s face and extend to below the chin.
Employers should stress hand hygiene before and after handling all PPE. Employers in meat and poultry processing industries should continue to stay up to date on the most current guidance concerning PPE.
As part of their hazard assessments, employers must always consider whether PPE is necessary to protect workers. Specifically, when engineering and administrative controls are difficult to maintain and there may be exposure to other workplace hazards, such as splashes or sprays of liquids on processing lines or disinfectants used for facility cleaning, PPE should be considered.
During the COVID-19 pandemic, meat and poultry processing employers should consider allowing voluntary use of filtering facepiece respirators (such as an N95, if available) for their workers, even if respirators are not normally required.
In addition to face shields as noted above, workers in meat and poultry processing facilities may need PPE such as gloves, face and eye protection, and other types of PPE when cleaning and disinfecting meat and poultry processing plants (including frequently touched surfaces), tools, and equipment.
When PPE is needed, employers should consider additional hazards created by poorly fitting PPE (e.g., mask ties that dangle or catch, PPE that is loose and requires frequent adjustment or tends to fall off) with respect to the work environment (e.g., machinery in which PPE could get caught).
Workers’ rights
Section 11(c) of the Occupational Safety and Health Act of 1970, 29 USC 660(c), prohibits employers from retaliating against workers for raising concerns about safety and health conditions. Additionally, OSHA’s Whistleblower Protection Program enforces the provisions of more than 20 industry-specific federal laws protecting employees from retaliation for raising or reporting concerns about hazards or violations of various airline, commercial motor carrier, consumer product, environmental, financial reform, food safety, health insurance reform, motor vehicle safety, nuclear, pipeline, public transportation agency, railroad, maritime, securities, and tax laws. OSHA encourages workers who suffer such retaliation to submit a complaint to OSHA as soon as possible in order to file their complaint within the legal time limits, some of which may be as short as 30 days from the date they learned of or experienced retaliation. An employee can file a complaint with OSHA by visiting or calling his or her local OSHA office; sending a written complaint via fax, mail, or email to the closest OSHA office; or filing a complaint online. No particular form is required, and complaints may be submitted in any language.
OSHA provides recommendations intended to assist employers in creating workplaces that are free of retaliation and guidance to employers on how to properly respond to workers who may complain about workplace hazards or potential violations of federal laws. OSHA urges employers to review its publication Recommended Practices for Anti-Retaliation Programs.
1 Employers should evaluate the burdens and benefits of recording workers’ temperatures or asking them to complete written questionnaires. These types of written products become records that must be retained for the duration of the workers’ employment plus 30 years. See OSHA’s Access to Employee Exposure and Medical Records standard (29 CFR 1910.1020).





















.png)












No hay comentarios:
Publicar un comentario