
Drug-monitoring innovations help providers help their patients
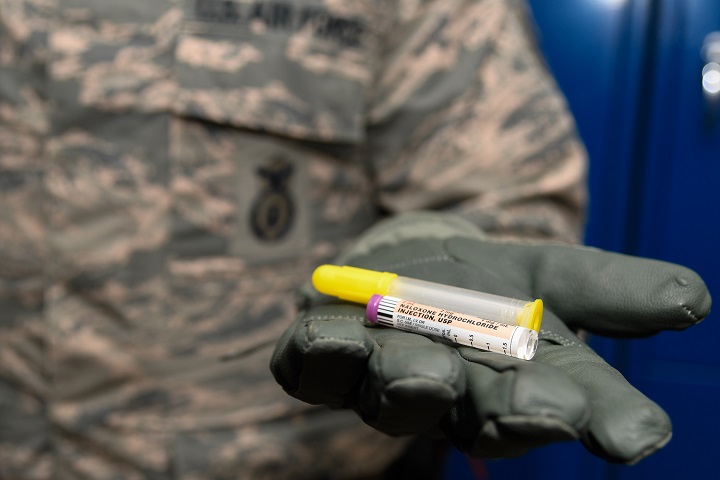
Two Military Health System innovations are helping to ensure best practices for patients with pain, and for patients who’ve been diagnosed with post-traumatic stress disorder. (U.S. Air Force photo by Senior Airman Curt Beach)
FALLS CHURCH, Va. — Two Military Health System innovations are helping to ensure best practices for patients with pain, and for patients who’ve been diagnosed with post-traumatic stress disorder.
The MHS Opioid Registry utilizes cutting-edge technology for data management and reporting to identify patients who’ve been prescribed opioids, said Chris Nichols, the Defense Health Agency’s program manager for Enterprise Intelligence and Data Solutions. Clinical pharmacy professionals, physicians, and other authorized providers can use the patient lookup capability to proactively monitor and manage patients, and intervene as appropriate.
Opioids such as oxycodone, hydrocodone, codeine, and morphine are prescribed to relieve pain. But they are highly addictive, health care experts say, and overuse can lead to death.
The rates of opioid addiction and overdose deaths are lower in the military than among the general population, said Vice Adm. Raquel Bono, DHA director, during a House Armed Service Committee hearing in June on Military Health System reform. Still, she said, the MHS has a role to play.
“Our beneficiaries are no strangers to chronic pain,” Bono said. “While our primary focus is on our own patient population, we’re also cognizant of the larger public health crisis surrounding opioids. As health professionals and public servants, we have an obligation to help confront that crisis.”
The MHS Opioid Registry was launched in December 2016 and released to all sites in 2017. Data in the registry includes more than 200 variables including demographics, medications, morphine equivalence daily dose, results of urine drug testing, and opioid risk factors. In the future, MHS Opioid Registry users will also be able to evaluate and track alternative non-opioid therapies for pain management.
Nichols said a registry that’s accessible by both DoD and VA providers and staff is currently under development.
The PTS Provider Prescribing Profile was developed by the DHA’s Pharmacy Operations Division. It lists all providers at military treatment facilities who are treating patients with PTSD or acute stress disorder, said Sushma Roberts, Ph.D., a clinical psychologist and senior program manager for DoD/VA Integrated Behavioral Health, Clinical Communities Support Section, Clinical Support Division. The tool also documents the medications providers are prescribing.
From February 2000 to June 2018, about 230,000 active-duty service members were diagnosed with PTSD, Roberts said, adding that 75 percent were diagnosed following a deployment of 30 days or longer.
The clinical practice guideline released in 2017 recommended against prescribing benzodiazepines for PTSD patients, Roberts said. Benzos, also known as tranquilizers, act on the brain and central nervous system to produce a calming effect. People can easily develop a tolerance to benzos, health care experts say, needing higher doses and increased frequency to achieve the same effects. People also may suffer withdrawal symptoms, including insomnia, irritability, anxiety, panic attacks, and seizures.
“Benzos aren’t necessarily bad,” said Army Lt. Col. Dennis Sarmiento, a psychiatrist and chair of the DHA’s Behavioral Health Clinical Community. “There are indications for their use. Short-term, they can help with anxiety, panic, and sleep. Treating such symptoms can help providers engage patients in care and better establish or reinforce rapport.”
But medications other than benzos are recommended for treating PTSD because they’re more effective, Sarmiento said. For example, antidepressants such as Zoloft, Paxil, Prozac, and Effexor raise the brain’s level of serotonin, a chemical that reduces symptoms of depression and anxiety.
They also can be used with trauma-focused psychotherapy, Sarmiento said. Those therapies include talking or writing about traumatic events, or learning and practicing meditation or deep-breathing exercises to manage anxiety.
Sarmiento notes that throughout the MHS, benzo prescriptions have been on a downward trend since peaking in 2012.
According to the tool, the number of benzos prescriptions for MHS beneficiaries diagnosed with PTSD dropped from 1,922 in the first quarter of fiscal year 2017 to 1,622 for second quarter of FY 2018.
Helping the healers through the power of mobile technology
Article
7/22/2018
App guards against emotional occupational hazards
Soldiers test Army's newest transport telemedicine technology
Article
7/20/2018

MEDHUB is really about life-saving situational awareness
Air Force, NASA seek potential medical collaboration
Article
7/19/2018

NASA and the military share a lot of similar medical issues
Navy Care app enables medical appointments from work, home
Article
7/13/2018

The app delivers convenient care with the quality of a face-to-face visit
DHA PI 6490.01: BH Treatment and Outcomes Monitoring
Policy
This Defense Health Agency-Procedural Instruction (DHA-PI), based on the authority of References (a) and (b), and in accordance with the guidance of References (c) through (k): a. Establishes the Defense Health Agency’s (DHA) procedures for the collection and analysis of BH outcome data. b. Addresses how DoD will standardize BH outcome data collection to: assess variations in mental health and substance use care among in-garrison medical treatment facilities (MTFs) and clinics; assess the relationship of treatment protocols and practices to BH outcomes; and identify barriers to provider implementation of evidence-based clinical guidance approved by DoD. c. Designates the Army as the DoD lead Service for maintenance and sustainment of the Behavioral Health Data Portal (BHDP) in specialty care mental health and substance use clinics, referred to collectively as BH clinics, until BHDP functionality can be integrated with GENESIS or another electronic health record (EHR) system managed by DHA. d. Designates DHA Information Operations (J-6) as lead on transitioning BHDP functional requirements related to outcomes monitoring to future EHR data collection platforms and processes.
- Identification #: DHA PI 6490.01
- Date: 7/12/2018
- Type: DHA Procedural Instruction
- Topics: Mental Health Care | Substance Abuse
There is hope
Article
7/11/2018

More than 350,000 deaths are attributed to opioid overdoses nationwide since 1999
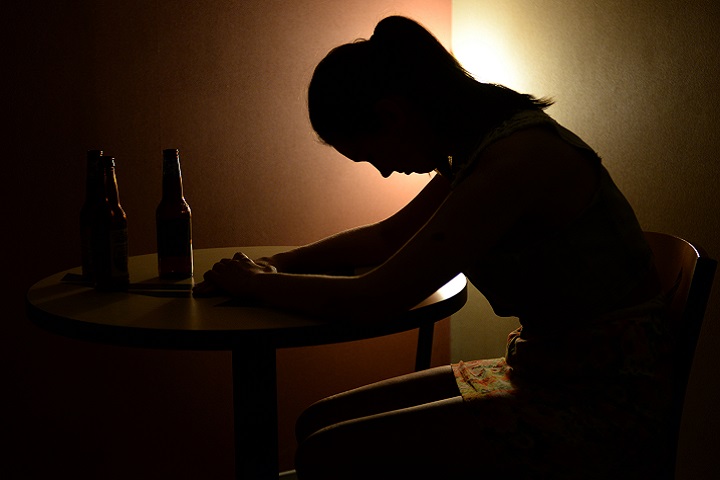
Life without liquor
Article
6/29/2018

One service member’s story of how he overcame a drinking problem
Progress in preventing opioid abuse, more needs to be done
Article
6/26/2018
The Military Health System has a shared responsibility in addressing the nation’s opioid epidemic
DHA PI 6025.04: Pain Management and Opioid Safety in the MHS
Policy
The purpose of our MHS Pain Management Campaign is to enable Clinical Communities to provide evidence-based pain management guided by clinical practice guidelines (CPGs): effectively treat acute and chronic pain; promote non-pharmacologic treatment; prevent acute pain from becoming chronic; and minimize use of opioids with appropriate prescribing only when indicated. The Pain Management Clinical Support Service achieves these ends through clinical improvements in pain care, clinician and patient education, and research. This Defense Health Agency-Procedural Instruction (DHA-PI) is a dual effort between the Pain Management Clinical Support Service and the Clinical Communities to achieve our stated purpose through implementation of the MHS Stepped Care Model.
- Identification #: DHA PI 6025.04
- Date: 6/8/2018
- Type: DHA Procedural Instruction
- Topics: TRICARE Pharmacy Program | Substance Abuse
Breaking down anxiety one fear at a time
Article
6/5/2018

Generalized anxiety, panic disorder, and anxiety related to PTSD are common disorders. In fact, an estimated 31 percent of U.S. adults experience anxiety at some point in their lives; one marine discusses his journey.
Military providers seek tailored approach to treating PTSD
Article
3/14/2018

New tool reviews, monitors provider prescribing habits
From an award ceremony to panel talks, senior leaders will have presence at HIMSS
Article
3/8/2018

Federal health, IT experts come together for discussion on hot topics
Traumatic Brain Injury and the Art of Paddling
Article
3/7/2018

A U.S. Army veteran’s recipe for embracing life after several TBIs
Air Force robotic surgery training program aims at improving patient outcomes
Article
2/9/2018

Robotic surgery is becoming the standard of care for many specialties and procedures
Seizures among Active Component service members, U.S. Armed Forces, 2007 – 2016
Infographic
1/25/2018

This infographic documents a retrospective study which estimated the rates of seizures diagnosed among deployed and non-deployed service members to identify factors associated with seizures and determine if seizure rates differed in deployment settings. The study also evaluated the associations between seizures, traumatic brain injury (TBI), and post ...


































No hay comentarios:
Publicar un comentario