
Highlights this issue
- Webinar featuring the 20th US Surgeon General, Acting CDC Director, and other clinical and public health professionals
March 13, 2018 from 2-3:30 pm EST
FREE Continuing Education (CE)
Hosted by: CDC’s Office for State, Tribal, Local, and Territorial Support (OSTLTS) and Clinician Outreach and Communication Activity (COCA)
Overview
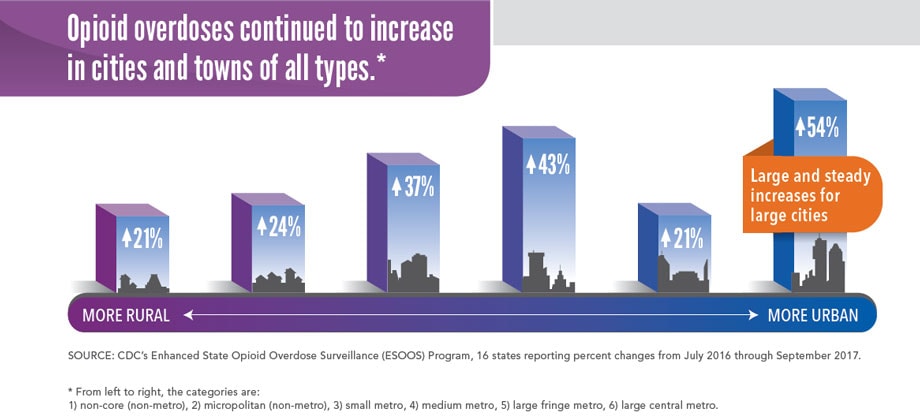
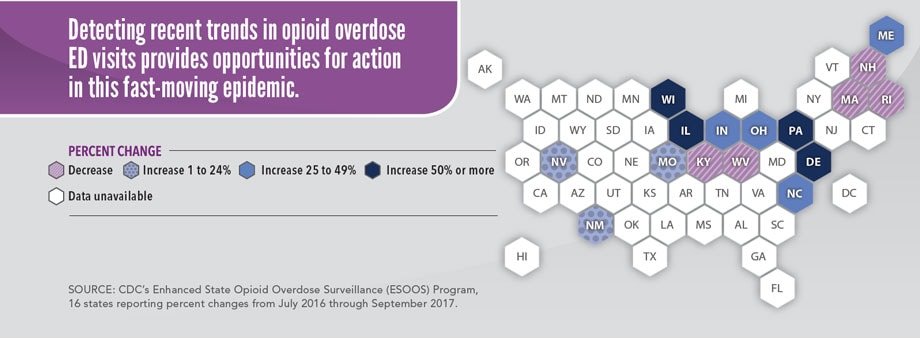
Emergency department (ED) visits for opioid* overdoses rose 30% in all parts of the US from July 2016 through September 2017. People who have had an overdose are more likely to have another, so being seen in the ED is an opportunity for action. Repeat overdoses may be prevented with medication-assisted treatment (MAT) for opioid use disorder (OUD), which is defined as a problematic pattern of opioid use. EDs can provide naloxone, link patients to treatment and referral services, and provide health departments with critical data on overdoses. ED data provide an early warning system for health departments to identify increases in opioid overdoses more quickly and coordinate response efforts. This fast-moving epidemic does not stay within state and county lines. Coordinated action between EDs, health departments, mental health and treatment providers, community-based organizations, and law enforcement can prevent opioid overdose and death.
Health departments can:
- Alert communities to rapid increases in overdoses seen in EDs for an informed and timely response.
- Increase naloxone distribution (an overdose-reversing drug) to first responders, family and friends, and other community members in affected areas, as policies permit.
- Increase availability of and access to treatment services, including mental health services and MAT for OUD.
- Support programs which reduce harms from injecting opioids, including those offering screening for HIV and hepatitis B and C, in combination with referral to treatment.
- Support the use of the CDC Guideline for Prescribing Opioids for Chronic Pain, which encourages using prescription drug monitoring programs (PDMPs) to inform clinical practice. https://go.usa.gov/xn6uQ
*Opioids include prescription pain medications, heroin, and illicitly manufactured fentanyl.

Problem
Opioid overdose ED visits continued to rise from 2016 to 2017.
From July 2016 through September 2017, opioid overdoses increased for:
- Men (↑30%) and women (↑24%)
- People ages 25-34 (↑ 31%), 35-54 (↑36%), and 55 and over (↑32%)
- Most states (↑ 30% average), especially in the Midwest (↑70% average)
SOURCE: CDC’s National Syndromic Surveillance Program, 52 jurisdictions in 45 states reporting.

View large image and text description





















.png)












No hay comentarios:
Publicar un comentario