- One in three people in the US will develop shingles—a painful rash disease—in their lifetime.
- CDC has updated its shingles vaccine recommendations: adults aged 50 or older should get the new, highly protective shingles vaccine called Shingrix.
- Healthcare professionals should recommend that patients aged 50 or older get two doses of Shingrix, 2 to 6 months apart.
Shingles Surveillance
Shingles and Postherpetic Neuralgia† Rates* by Age, United States
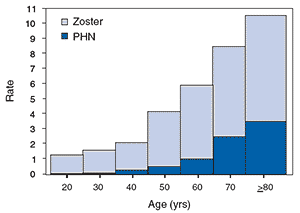
*per 1,000 person-years.
† Defined as pain for 30 days or longer
Source: https://www.cdc.gov/mmwr/preview
/mmwrhtml/rr5705a1.htm
† Defined as pain for 30 days or longer
Source: https://www.cdc.gov/mmwr/preview
/mmwrhtml/rr5705a1.htm
Almost 1 out of 3 people in the United States will develop shingles during their lifetime. Most people who get shingles will have it only once. However, it is possible to get it a second or even third time.
Your risk of getting shingles increases as you get older. The most common complication of shingles is postherpetic neuralgia (PHN), which is severe pain in the areas where the shingles rash occurred. About 10 to 15% of people who get shingles will experience PHN. The risk of PHN increases with age.
Children can get shingles, but it is not common.
Hospitalizations
Approximately 1 to 4% of people who get shingles are hospitalized for complications. Older adults and people with weakened or suppressed immune systems are more likely to be hospitalized. About 30% of people hospitalized for shingles have a weakened or suppressed immune system.
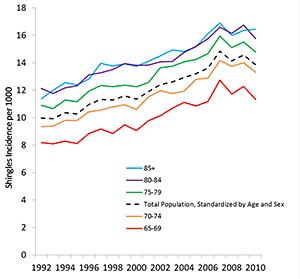
Trends
Shingles is increasing among adults in the United States. The increase has been gradual over a long period of time. We do not know the reason for this increase.
One popular explanation, now thought unlikely, is that the increase in shingles might be related to fewer chickenpox cases in United States children due to widespread vaccination against chickenpox. Some people suggest that chickenpox boosts a person’s immunity to the varicella-zoster virus (VZV) and reduces the risk of VZV reactivating as shingles. Therefore, less children with chickenpox could theoretically lead to an increase in shingles in adults. However, this proposed explanation seems unlikely based on two CDC studies which found that shingles rates:
- started increasing before chickenpox vaccine was introduced in the United States, and
- did not increase faster after the routine chickenpox vaccination program started.
Other countries without routine chickenpox vaccination programs, have observed similar increases in shingles rates.
Although not common among children, the rate of shingles in United States children has been declining since the routine varicella vaccination program began. Like the wild-type (natural) virus, the attenuated (weakened) vaccine virus can reactivate and cause shingles. However, children who get the chickenpox vaccine appear to have a much lower risk of shingles than children who were infected with wild-type chickenpox. Vaccinated children are less likely to become infected with wild-type chickenpox virus, which is more likely to reactivate as shingles compared to attenuated vaccine virus.
Shingles Vaccination
In 2015, 31% of adults 60 years and older reported receiving Zostavax®, a shingles vaccine in use since 2006. This is an increase from the 28% reported the previous year.
CDC will begin collecting data on vaccination of adults 50 years and older using Shingrix, and will share this information when it is available.
References
- Hales CM, Harpaz R, Joesoef MR, Bialek SR (2013). Examination of links between herpes zoster incidence and childhood varicella vaccination.Annals of Internal Medicine. 159(11):739-45.
- Weinmann S, Chun C, Schmid DS, Roberts M, Vandermeer M, Riedlinger K, et al. Incidence and clinical characteristics of herpes zoster among children in the varicella vaccine era, 2005–2009.Journal of Infection Diseases. 2013;208(11):1859-68.
- Mahamud A, Marin M, Nickell SP, Shoemaker T, Zhang JX, Bialek SR. Herpes zoster-related deaths in the United States: validity of death certificates and mortality rates, 1979-2007. Clin Infect Dis.2012 Oct;55(7):960-6.
- Leung J, Harpaz R, Molinari NA, Jumaan A, Zhou F. Herpes zoster incidence among insured persons in the United States, 1993-2006: evaluation of impact of varicella vaccination. Clinical Infectious Diseases. 2011;52(3):332-340.
- Jumaan AO, Yu O, Jackson LA, Bohlke K, Galil K, Seward JF. Incidence of herpes zoster, before and after varicella vaccination-associated decreases in the incidence of varicella. Journal of Infectious Diseases. 2005;191:2002-7.
- Brisson M, Edmunds WJ, Law B, et al. Epidemiology of varicella zoster virus infection in Canada and the United Kingdom. Epidemiol Infect2001;127,305–14.
- Schmader K. Herpes zoster in older adults. Clin Infect Dis 2001;32:1481–6.





















.png)












No hay comentarios:
Publicar un comentario