
Chromosomal Instability Score May Predict Response to Cancer Treatment
September 23, 2016 by NCI Staff
A team led by researchers from the Lawrence Berkeley National Laboratory has identified a new type of biomarker that may help predict prognosis and response to chemotherapy and radiation therapy for several types of cancer.
The biomarker is a score based on theexpression levels of a set of genes involved in partitioning chromosomes during cell division. This score, the researchers found, could identify tumors that would likely not respond to certain treatments and those that would be sensitive. The score could also predict patients’ outcomes with or without treatment.
The study was published August 31 in Nature Communications.
Cellular Machinery Gone Awry
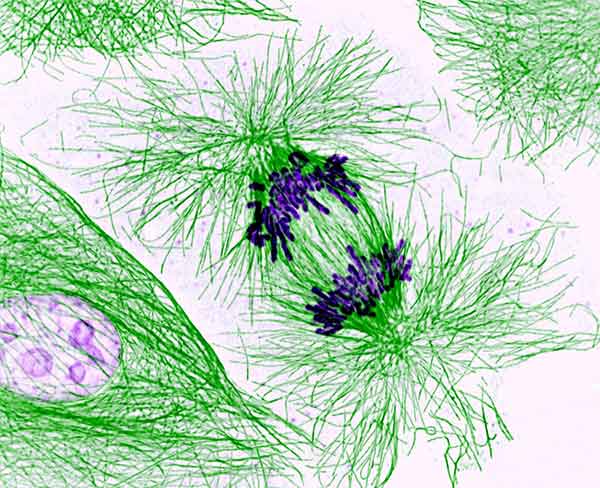
In a dividing cell, the centromere and kinetochore are parts of the cellular machinery that pull the duplicated chromosomes apart into two new daughter cells. If something goes awry during this process, a cell can end up with too many chromosomes, with too few chromosomes, or with rearranged chromosomes. Any of these outcomes—known collectively as chromosomal instability—have the potential to drive cancer.
Researchers in the lab of Gary Karpen, Ph.D., wanted to know whether changes in the expression of genes associated with normal centromere and kinetochore function contribute to chromosomal instability, and, if so, whether these changes might provide important information about the behavior of a tumor.
So a research team led by Weiguo Zhang, Ph.D., and Jian-Hua Mao, Ph.D., picked 31 genes that previous studies had shown are involved in centromere and kinetochore assembly. Using large tumor gene-expression databases, they first examined the expression levels of these genes in different cancer types. Many of these genes were over- or under-expressed in many of the tumors compared with corresponding normal tissues, and these changes in expression differed substantially both across cancer types and among people with the same cancer type.
Using another set of databases containing thousands of samples from breast, lung, ovarian, and gastric cancers, the researchers then determined that levels of over-expression of 14 of the original 31 genes were significantly associated with risk of disease progression and survival.
Dubbing the expression of this 14-gene subset the Centromere and kinetochore gene Expression Score (CES), they measured the CES in samples from The Cancer Genome Atlasand other tumor sample databases. A high CES, they found, correlated significantly with elevated chromosomal instability of tumors from many cancer types, and with tumor features that are associated with poor prognosis in several cancer types, such as overexpression of the HER2 protein in breast cancer.
High Instability, High Sensitivity
To determine if the CES could help predict outcomes and survival, the research team measured the score in several large gene-expression datasets from patients with breast or lung cancer for whom the treatment outcomes were known.
They divided patients into high-, medium-, and low-CES groups, and found that patients in the high-CES group had the worst outcomes. Similarly, when they looked at another dataset from patients with early-stage non-small cell lung cancer or ovarian cancer, those with the highest CES had the worst outcomes. The association between CES and outcome was independent of other prognostic factors, including tumor stage and grade, breast cancer hormone-receptor status, and lung cancer subtype.
Because cancer cells with a high CES have already experienced substantial disruption of their genetic material, the researchers tested whether high CES could predict increased sensitivity to chemotherapy or radiation therapy, two treatments that cause DNA damage. Indeed, in their initial studies of cancer cell lines, those with a high CES experienced more cancer cell death when exposed to chemotherapeutic agents (such asirinotecan) compared to cell lines with a low CES.
Patient samples yielded similar results. In lung cancer samples taken from patients in a clinical trial that had tested chemotherapy versus no adjuvant treatment for early-stage lung cancer, patients with a high CES who had received chemotherapy had significantly improved survival compared with those who did not, whereas patients with a low CES gained no significant survival benefit from adjuvant chemotherapy.
And among patients with estrogen receptor positive breast cancer, those with a high CES who received chemotherapy had a reduced risk of the cancer returning, similar to rates for patients with a low CES and lower than for patients with a high CES who did not receive chemotherapy. Similar results were obtained for adjuvant radiation therapy in patients with breast cancer or lung cancer.
Making Decisions with More Precision
A low CES in a patient potentially “could be used to rule out the use of inappropriate and ineffective drugs, in favor of different treatment approaches,” commented Julia Cooper, Ph.D., head of the Telomere Biology Section in NCI’s Center for Cancer Research, who was not involved in the study.
Because cells with centromere factor misregulation appear to be much more sensitive to treatments that damage DNA, Dr. Cooper continued, the CES could also potentially be used to identify patients who could be treated with lower doses of these drugs, reducing the risk of side effects.
The CES may also be able to identify patients who would benefit from the addition of a drug that enhances the efficacy of DNA-damaging therapies, added Dr. Karpen.
Exploring such clinical uses would require a validated, easily reproducible test that can be used on fresh or stored tumor samples, explained Dr. Karpen. His team is working on developing such a test, and is partnering with clinicians in the United States and China to verify the test’s predictive power in tumor samples from well-controlled clinical trials.
He and his colleagues also want to test further whether the CES can distinguish early stage growths that will not become invasive or metastatic, such as indolent breast ductal carcinoma in situ (DCIS), which may not benefit from first-line therapy.
“We don’t always know which treatments are best for which cancers,” Dr. Karpen said. “If a treatment is not going to be effective, you run the risk of serious side effects” without providing any benefit to the patient.
Their goal, he said, is to develop tests “that allow both patients and physicians to make these decisions with more precision.”






















.jpg)












No hay comentarios:
Publicar un comentario