Clot Removal: Impressive Results for Stent Retrievers in Acute Stroke
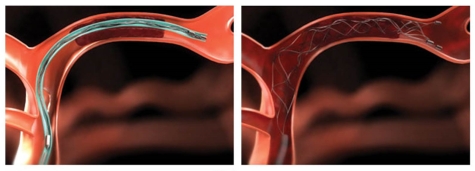
Caption: Schematic of how the clot retriever used in the reported trials is opened inside a blood vessel to surround a clot that is blocking blood flow. Once caught by the stent, the entire apparatus with the clot is removed from the body out a small puncture in the femoral artery at the groin.
Credit: Covidien
Credit: Covidien
Despite the recent progress we’ve made in preventing stroke by such steps as controlling weight, lowering blood pressure, and stopping smoking, nearly 700,000 Americans suffer clot-induced, or ischemic, strokes every year [1]. So, I’m very pleased to report that, thanks to years of rigorous research and technological development, we’ve turned a major corner in the emergency treatment of this leading cause of death and disability.
The most severe strokes—those that can cause lifelong loss of independent function—are often due to blood clots that suddenly enter and block one of the main arteries supplying blood flow to the brain. No less than four large, randomized clinical trials recently reported results showing, for the first time, that using catheters to remove large clots from cerebral arteries can restore blood flow and halt further damage to the brains of patients with acute strokes. In fact, the stent-based retrievers and other mechanical approaches used to remove stroke-causing clots proved so effective, that three of the four trials were stopped early, allowing the results to be made swiftly available to medical professionals and the public.
This is potentially great news for people who suffer the onset of severe ischemic strokes and their loved ones. All of the studies found that clot-removal procedures, also referred to as endovascular therapy, shortened stroke patients’ recovery times by at least a few months and significantly improved their chances of regaining independence.
Still, it’s important to keep in mind that, as for most other stroke treatments, clot-removal procedures involve a race against the clock. The researchers found that to prevent brain damage from becoming too widespread (an estimated 2 million brain cells die per minute during a severe stroke), a clot must be removed within hours of the first stroke symptoms—the earlier, the better.
Currently, most people arriving in the emergency room with an ischemic stroke will be evaluated to see if the clot can be dissolved by a drug called tissue plasminogen activator (tPA) that is injected into a vein. However, tPA must be administered within 3 to 4.5 hours of an acute stroke, and isn’t effective in breaking down large clots more than half of the time.
The search for a better way to remove large clots has spurred efforts to develop endovascular therapies that can remove such clots by mechanical means. Most of the procedures developed over the past few decades work in this way: doctors puncture the femoral artery near the groin, insert a catheter into the artery, and thread the catheter up through vascular system to the artery that feeds the brain. So far, so good. However, once inside the brain artery, there have been major challenges over the years in developing effective technology to remove those stroke-causing clots.
Numerous experimental “clot extractors” were devised to tackle the job. The newest generation devices are “stent retrievers,” which resemble the wire stents often used to keep open coronary arteries, but actually function more like a trap. When a catheter containing a collapsed stent retriever reaches a clot blocking a cerebral artery, the stent moves out of the catheter, unfolds to form a 3D mesh tube, ensnares the clot, and retracts back into catheter with its catch. Researchers then thread the catheter with the clot back out of the body. Meanwhile, the artery is cleared, allowing blood to flow back into the brain and replenish its vital supply of oxygen and glucose.
In 2011, the first large clinical trials of clot retrievers reported their results. The results were disappointing—all showed no benefit to patients. But those studies primarily evaluated first-generation clot retrievers. Unwilling to give up, some researchers went on to design trials for second-generation stent retrievers, which are faster and more flexible.
As the new results show, the researchers’ hunches were right on target. The first finding came from The Netherlands and a 500-patient study known as MR. CLEAN [2]. Researchers found that one in five patients who were treated with tPA alone recovered enough after their strokes to live independently. For those who received tPA plus endovascular therapy, primarily with a stent retriever, one in three returned to independence.
Next came a three-continent study with 316 patients known by the acronym ESCAPE [3]. The study was stopped early because its preliminary data unequivocally confirmed the results of the MR. CLEAN trial. The same was true for the 70-patient EXTEND-IA trial, conducted in Australia and New Zealand [4]. This NIH co-supported study, also halted early, showed that patients treated with a combination of tPA and endovascular therapy using a stent retriever had superior outcomes compared to those who received tPA alone. Those outcomes included restored blood flow to the brain, quicker recovery time, and a return to independence.
In February, the international SWIFT PRIME study weighed in with its preliminary analysis of its first 200 patients. Sixty percent of those treated with tPA and endovascular therapy using a stent retriever lived independently, compared to 35 percent who received tPA alone. Or, to put these numbers in better perspective: For every 100 stroke patients, 39 had less disability because of endovascular therapy.
Another critical factor must be mentioned here. These studies are among the first to incorporate rapid imaging of the brain’s vascular physiology. The doctors incorporated non-invasive CT and MRI imaging of the brain blood vessels to select patients with clots that were treatable by endovascular therapy. Comparison maps of brain blood flow and injury also allowed doctors to select only the patients whose brain injury remained limited enough to still benefit from removing the clot.
“Time is brain” in acute stroke treatment. In these studies, the care teams got really good at beating the clock. In the EXTEND-IA trial, which involved multiple study sites, the researchers found that acquiring, processing, and interpreting images was largely dependent on the speed of the available computer network, not necessarily the interactions of hospital staff. They found the imaging typically could be obtained in under 15 minutes. In SWIFT PRIME, the picture-to-procedure rate was 58 minutes. In the ESCAPE trial, it took on average 83 minutes from picture to the clot retrieval procedure.
The challenge for the health care community will now be translating the impressive results of these studies into systems of stroke care all across this nation and around the world. If successful, many more patients will be helped, and the functional benefit will be even more substantial. In the video featured in the first link below, Dr. Walter Koroshetz, the acting director of NIH’s National Institute of Neurological Disorders and Stroke Walter, offers his perspectives—be sure to take a look.
As for the public, the best thing you can do is to know the signs of stroke and call 911 immediately if you or a loved one happen to experience them. Most people know about the importance of getting immediate treatment for a heart attack. The same urgency must now be applied to seek medical care for a “brain attack,” a stroke. The signs are:
- Sudden NUMBNESS or weakness of face, arm, or leg, especially on one side of the body
- Sudden CONFUSION, trouble speaking or understanding speech
- Sudden TROUBLE SEEING in one or both eyes
- Sudden TROUBLE WALKING, dizziness, loss of balance or coordination
- Sudden SEVERE HEADACHE with no known cause
References:
[1] Executive summary: heart disease and stroke statistics—2015 update: a report of the American Heart Association. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, et al. Circulation. 2015 Jan 27: 131(4):434-441.
[2] A randomized trial of intraarterial treatment for acute ischemic stroke. Berkemer OA, Fransen PSS, Dippel DWJ et al. NEJM, 2015 Jan 1;372(1):11-20.
[3] Randomized assessment of rapid endovascular treatment of ischemic stroke. Goyal M, Demchuk BK, Hill MD, et al. NEJM, 2015 Feb 11;DOI:10.1056
[4] Endovascular therapy for ischemic stroke with perfusion-imaging selection. Campbell BCV, Mitchell PJ, Davis SM et al. NEJM, 2015 Feb 11[Epub ahead of publication]
Links:
Video: NINDS Acting Director Walter Koroshetz on New Therapy for Acute Stroke (National Institute of Neurological Disorders and Stroke/NIH)
Stroke Information Page (National Institute of Neurological Disorders and Stroke/NIH)
The Internet Stroke Center (supported in part by NIH grants)
NIH Stroke Scale (assessment tool to measure stroke-related neurological decline)
Covidien Revascularization Device Receives FDA Clearance (press release, including video showing how one type of stent retriever works)
NIH Support: National Institute of Neurological Disorders and Stroke


































No hay comentarios:
Publicar un comentario