
Joint Staff doctor explains TBI diagnosis procedures

An Airman searches for salvageable items after missile attacks at Al Asad Air Base, Iraq, Jan. 12, 2020. At a Pentagon news conference, Air Force Brig. Gen. (Dr.) Paul Friedrichs, the Joint Staff Surgeon, said 110 service members have been diagnosed with mild traumatic brain injuries from the attack. Most have returned to duty, while 25 returned to the United States for further treatment, he said, and six more are still undergoing testing. (U.S. Army photo by Spc. Derek Mustard)
WASHINGTON — Traumatic brain injuries can't be quickly diagnosed – as was the case with the Iranian missile attack on Al Asad Air Base in Iraq on Jan. 8, the Joint Staff surgeon said.
At a Pentagon news conference today, Air Force Brig. Gen. (Dr.) Paul Friedrichs, the Joint Staff Surgeon, said 110 service members have been diagnosed with mild traumatic brain injuries from the attack. Most have returned to duty, while 25 returned to the United States for further treatment, he said, and six more are still undergoing testing.
Following an attack, commanders assess injuries, Friedrichs said, and in this case, no one immediately appeared to have had acute injuries. "No one lost a leg, no one lost an eye, no one lost a limb – which was remarkable given the strength of these munitions," the doctor said.
Therefore, he explained, reports went up the chain of command saying no one had an acute injury. But a TBI takes time to diagnose, and the process is involved. Protocols call for TBI testing of service members who were within 50 meters of an explosion, were exposed to a series of explosions, had a direct blow to the head, or who exhibit symptoms such as headache, dizziness, memory problems, balance problems, nausea, vomiting, difficulty concentrating, irritability and visual disturbance.
The tests take up to two days to complete. But service members may have TBI and feel they can power through and just go back to duty. They may have symptoms, but they don't go away and may get worse, Friedrichs said.
"A lot of people have said, 'Well, why didn't we immediately identify everybody with a traumatic brain injury?'" the general said. "[It's] because the signs sometimes are fairly nonspecific. And … even though we've trained everybody who deploys downrange on what to look for, it's quite common that we'll have folks who will say, 'I just was blasted. Of course, I'm not going to feel quite right. I'm going to ride this out for a few days.' Or 'I'm going to wait and see if this gets better.' And then they come in several days or weeks after the fact."
While there are tests that can point to TBI, some cases also require an MRI. The closest MRI testing facility to Iraq is in Germany, adding to the delay in diagnosis.
The department takes TBI extremely seriously, the doctor said, and has invested $1.5 billion in diagnosing and treating the condition. Test groups are wearing sensors to measure blast effects that could give medical professionals better information when making diagnoses, he noted.
"I think that's going to be really exciting going forward because that takes some of the subjectivity out," he said. "There is no military in the world that has invested as much or has fielded as many evidence-based tools as what we have right now."
Disclaimer: Re-published content may be edited for length and clarity. Read original post.
Positive attitude, social support may promote TBI/PTSD resilience
Article
7/23/2019

Psychological experiences prior to an injury may play a role in recovery
Warm Handoff for Transitioning Servicemembers Suffering from PTSD and TBI
Congressional Testimony
7/8/2019
S. 2987, SASC Report for FY 2019, 115-262, Pg. 203-204
New clinical recommendations on cognitive rehabilitation for TBI released
Article
6/24/2019

Cognitive rehabilitation focuses on improving thinking and communication skills
Chronic Traumatic Encephalopathy (CTE)
Congressional Testimony
6/13/2019
H.R. 5515 HASC Report for FY 2019 115-676, Pg. 128
Medical museum features mask-making arts therapy exhibit
Article
4/5/2019
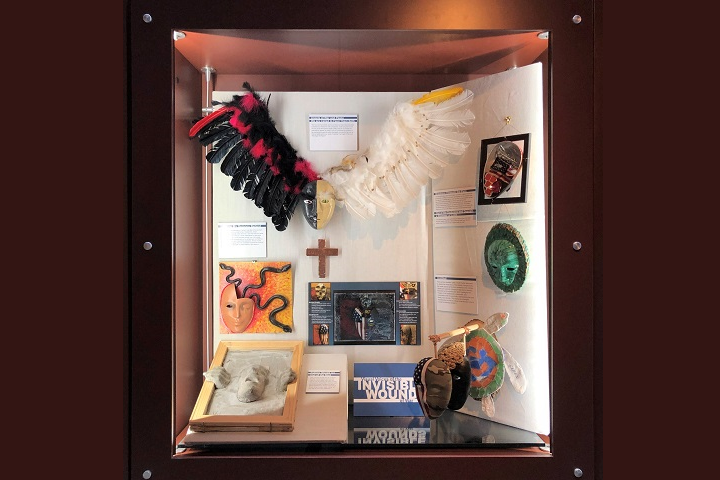
The exhibit explores the psychosocial environment of patients with TBI
Emerging technology improves ability to see ‘invisible’ wounds
Article
3/29/2019

Ultimate goal is better understanding, quality of life for warfighters
The National Intrepid Center of Excellence promotes warfighter brain health during Brain Injury Awareness Month
Article
3/28/2019

For the fifth year, the NICoE hosted a TBI resource fair at Walter Reed National Military Medical Center
Traumatic brain injury: Stories of strength and resilience
Article
3/19/2019

Not everyone with a TBI experiences the same signs and symptoms
Defense and Veterans Brain Injury Center releases new concussion screening tool
Article
3/15/2019

Providers who screen patients for concussion now have a new and improved tool
Concussion: Know the Symptoms
Video
3/12/2019

A racquetball game goes wrong when one player slips and hits his head. He thinks he's OK and his partner isn’t sure what to do about it.
DoD recognizes Brain Injury Awareness month, promotes warfighter brain health
Article
3/1/2019

Traumatic Brain Injury is a signature injury of current conflicts
Traumatic Brain Injury/Psychological Health
Congressional Testimony
1/25/2019
S. 3000, SAC Report for FY 2017, 114-263, Pg. 193
Promoting better understanding, treatment of traumatic brain injury
Article
12/26/2018

Blood test to identify TBI among 2018 achievements
Pilot Program on Investigational Treatment of Members of the Armed Forces for TBI and PTSD
Congressional Testimony
10/9/2018
HR 3304, NDAA for FY 2014, Sec. 704
Labyrinth: This path is made for mindful walking
Article
9/27/2018

NICoE uses ancient symbol to promote healing





















.png)












No hay comentarios:
Publicar un comentario