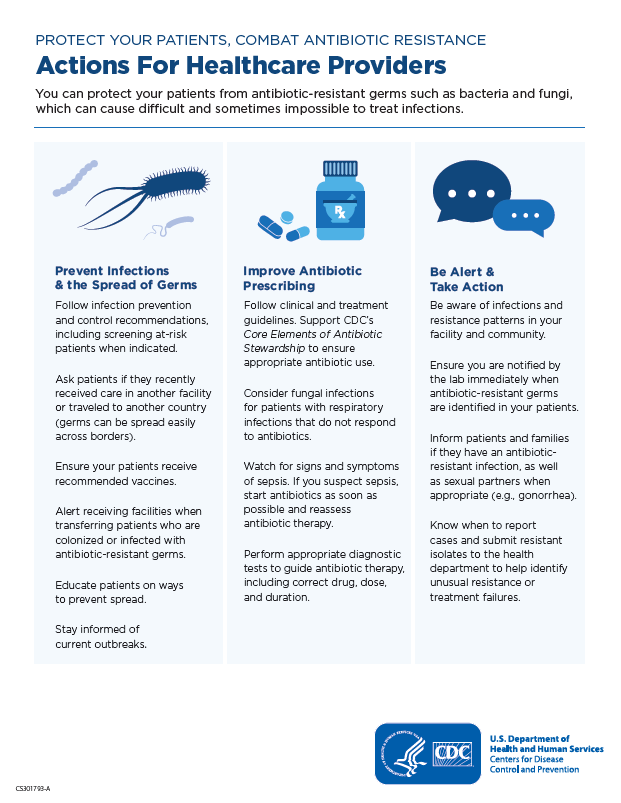
Protecting Patients and Stopping Outbreaks
On This Page
Your patients can get infections when receiving healthcare, called healthcare-associated infections (HAIs). HAIs are commonly caused by antibiotic-resistant pathogens (harmful germs), which may lead to sepsis or death. People can also get antibiotic-resistant infections in their community, for example, gonorrhea, tuberculosis (TB), or foodborne infections.
Take the following actions to help protect your patients and people in the community from antibiotic-resistant infections.
Help Prevent Infections and their Spread
- Follow infection prevention and control guidelines (including screening at-risk patients when indicated):
- Ask patients if they have recently received care in another facility or traveled to another country (germs can spread easily across borders).
- Ensure your patients receive recommended vaccines, and talk to them and their families about:
- Preventing infections
- Keeping scrapes and wounds clean
- Managing chronic conditions
- Seeking medical care when an infection is not getting better
- Understanding when antibiotics are needed
- Alert the receiving facility when transferring patients who are colonized or infected with antibiotic-resistant germs, and ask colleagues to use an Inter-Facility Infection Control Transfer Form [PDF – 3 pages]
- Educate patients on ways to prevent spread
- Stay informed of current outbreaks

Improve Antibiotic Prescribing
Antibiotics save lives, but any time they are used it can cause side effects and lead to antibiotic resistance.
- Follow clinical and treatment guidelines. Support CDC’s Core Elements of Antibiotic Stewardship to ensure appropriate antibiotic use
- Consider fungal infections for patients with respiratory infections that do not respond to antibiotics, for example:
- Valley fever (coccidioidomycosis)
- Histoplasmosis
- Blastomycosis
- Watch for signs and symptoms of sepsis: Clinical Resources and Guidelines
- Perform appropriate diagnostic tests to guide antibiotic therapy, including correct drug, dose, and duration
- Optimize TB therapy: Treatment for TB Disease
Be Alert and Take Action
- Be aware of infections and resistance patterns in your facility and community
- Ensure you are notified by lab immediately when antibiotic-resistant germs are identified in your patients
- Inform patients and families if they have an antibiotic-resistant infection, as well as sexual partners when appropriate (e.g. gonorrhea)
- Know when to report cases and submit resistant isolates to the health department to help identify unusual resistance or treatment failures
- For example, report gonorrhea isolates with decreased cephalosporin susceptibility or clinical treatment failure to CDC through your state or local public health authority


































No hay comentarios:
Publicar un comentario