01/17/2020 04:47 PM EST
Source: Centers for Disease Control and Prevention
Related MedlinePlus Pages: Antibiotic Resistance
Related MedlinePlus Pages: Antibiotic Resistance
About Antibiotic Resistance
Antibiotic resistance happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. That means the germs are not killed and continue to grow.
Infections caused by antibiotic-resistant germs are difficult, and sometimes impossible, to treat. In most cases, antibiotic-resistant infections require extended hospital stays, additional follow-up doctor visits, and costly and toxic alternatives.
Antibiotic resistance does not mean the body is becoming resistant to antibiotics; it is that bacteria have become resistant to the antibiotics designed to kill them.
Antibiotic Resistance Threatens Everyone
Terms
On CDC’s website, antibiotic resistance is also referred to as antimicrobial resistance or drug resistance.
Antibiotic resistance has the potential to affect people at any stage of life, as well as the healthcare, veterinary, and agriculture industries, making it one of the world’s most urgent public health problems.
Each year in the U.S., at least 2.8 million people are infected with antibiotic-resistant bacteria, and more than 35,000 people die as a result.
No one can completely avoid the risk of resistant infections, but some people are at greater risk than others (for example, people with chronic illnesses). If antibiotics lose their effectiveness, then we lose the ability to treat infections and control public health threats.
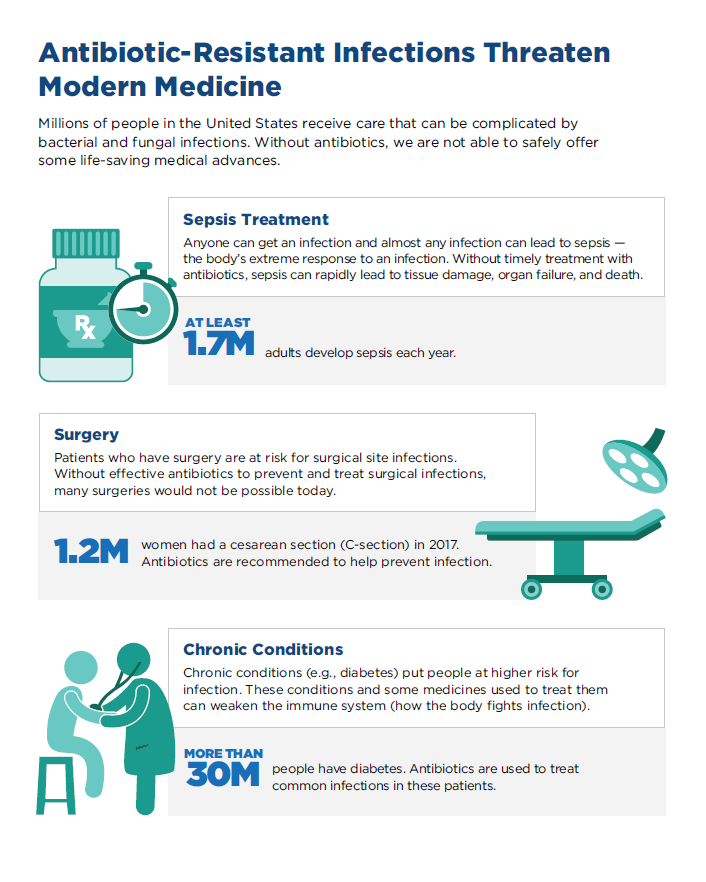
Many medical advances are dependent on the ability to fight infections using antibiotics, including joint replacements, organ transplants, cancer therapy, and treatment of chronic diseases like diabetes, asthma, and rheumatoid arthritis.
Brief History of Resistance and Antibiotics
Learn how CDC is leading efforts to combat antibiotic resistance through the Antibiotic Resistance Solutions Initiative.
Penicillin, the first commercialized antibiotic, was discovered in 1928 by Alexander Fleming. Ever since, there has been discovery and acknowledgement of resistance alongside the discovery of new antibiotics. In fact, germs will always look for ways to survive and resist new drugs. More and more, germs are sharing their resistance with one another, making it harder for us to keep up.
Select Germs Showing Resistance Over Time
| Antibiotic Approved or Released | Year Released | Resistant Germ Identified | Year Identified |
|---|---|---|---|
| Penicillin | 1943 | Penicillin-resistant Streptococcus pneumoniae Penicillinase-producing Neisseria gonorrhoeae | 1967 1976 |
| Vancomycin | 1958 | Plasmid-mediated vancomycin-resistant Enterococcus faecium Vancomycin-resistant Staphylococcus aureus | 1988 2002 |
| Amphotericin B | 1959 | Amphotericin B-resistant Candida auris | 2016 |
| Methicillin | 1960 | Methicillin-resistant Staphylococcus aureus | 1960 |
| Extended-spectrum cephalosporins | 1980 (Cefotaxime) | Extended-spectrum beta-lactamase- producing Escherichia coli | 1983 |
| Azithromycin | 1980 | Azithromycin-resistant Neisseria gonorrhoeae | 2011 |
| Imipenem | 1985 | Klebsiella pneumoniae carbapenemase (KPC)-producing Klebsiella pneumoniae | 1996 |
| Ciprofloxacin | 1987 | Ciprofloxacin-resistant Neisseria gonorrhoeae | 2007 |
| Fluconazole | 1990 (FDA approved) | Fluconazole-resistant Candida | 1988 |
| Caspofungin | 2001 | Caspofungin-resistant Candida | 2004 |
| Daptomycin | 2003 | Daptomycin-resistant methicillin-resistant Staphylococcus aureus | 2004 |
| Ceftazidime-avibactam | 2015 | Ceftazidime-avibactam-resistant KPC-producing Klebsiella pneumoniae | 2015 |
Find more information on the development of antibiotic resistance in the latest AR Threats Report.



































No hay comentarios:
Publicar un comentario