
Moving Beyond BMI: Low Muscle Mass May Affect Cancer Survival
April 30, 2018, by NCI Staff
For some women diagnosed with breast cancer, low muscle mass may be linked with a poor long-term prognosis, a new study has found.
In one of the largest investigations of its kind conducted to date, researchers found that one-third of the women included in the study had low levels of skeletal muscle mass—a condition known as sarcopenia—at the time of their diagnosis. And having low levels of muscle mass was associated with a higher risk of dying compared with women who had adequate muscle mass, the researchers reported April 5 in JAMA Oncology.
All of the women included in the study had breast cancer that had not yet spread beyond the breast at the time their cancer was diagnosed. The high proportion of women in the study with sarcopenia suggests that low muscle mass “is underappreciated” in women with earlier-stage breast cancer, said the study's lead investigator Bette Caan, Dr.P.H., of the Kaiser Permanente of Northern California Division of Research. The study also suggests that low muscle mass is as prevalent in patients “and is as strongly associated with decreased survival" as high levels of fatty tissue, or high adiposity, she continued.
In a similar study led by Dr. Caan, sarcopenia at diagnosis also was linked with worse survival in people with nonmetastatic colorectal cancer.
According to Joanne Elena, Ph.D., M.P.H., of NCI's Division of Cancer Control and Population Sciences, these studies are adding to the growing evidence that “low muscle mass may be another way to help identify patients at an increased risk for poor outcomes."
Unraveling the "Obesity Paradox"?
Obesity is now firmly recognized as an important risk factor for a host of cancers, and some studies have suggested that it can also increase the risk of death in those diagnosed with certain cancers.
But there are some anomalies in the data.
Some studies, in fact, have found that leaner people diagnosed with several different cancer types have a higher risk of dying than those who, according to their body-mass index body mass index (BMI), are overweight or mildly obese. Similar findings have been reported in diseases other than cancer, and the phenomenon has come to be known as the "obesity paradox"—the idea that having some excess body fat offers a measure of protection against disease-related death.
Researchers typically measure BMI as an umbrella measure of body composition "because it is relatively easy to collect in large studies," wrote Elisa Bandera, M.D., Ph.D., of the Rutgers Cancer Institute and Esther John, Ph.D., of the Stanford University School of Medicine in an editorial that accompanied the new study.
"BMI is an easy clinical tool that we can all use," said Grant Williams, M.D., of the Institute of Cancer Outcomes and Survivorship at the University of Alabama Birmingham Comprehensive Cancer Center. "But at same time, it misses a lot of the intricacies of body composition."
Given the limitations of BMI, researchers have wondered whether excess fat is actually protective, or if there are other aspects of body composition, including a lack of muscle, that might explain these paradoxical findings.
"Muscle is an independent organ, the largest organ in the body," Dr. Caan explained. Just like fat tissue, she continued, it is involved in functions such as the secretion of hormones, like insulin, and influences biological processes like metabolism and inflammation.
"The independent role of muscle is underappreciated," she said.
Using CT Scans to Provide Important Information
The approximately 3,200 women in the NCI-funded, retrospective study were diagnosed at Kaiser Permanente or Dana-Farber Cancer Institute between 2000 and 2013.
All of the women underwent pelvic or abdominal computed tomography (CT) scans within 6 months of being diagnosed with breast cancer—which is routinely done to ensure the cancer has not spread—but before beginning any active treatment. None of the women had very early breast cancer (stage 0 or 1), because CT scans aren’t typically performed in such patients.
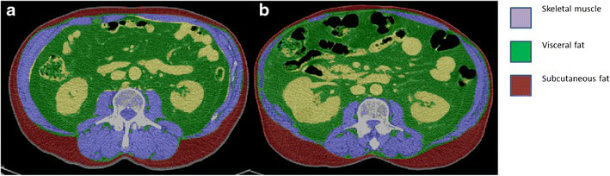
Dr. Caan and her colleagues used information from the CT scans to determine the patients’ muscle mass as well as their total adiposity, which was defined as the cumulative amount of the three different types of fat tissue. They also calculated patients' BMI.
Women who had sarcopenia at diagnosis had a moderately increased risk (approximately 40%) of dying from any cause, not just cancer, during the study period than women without sarcopenia, the researchers found. Women who had high adiposity had a similarly increased risk (35%) of dying, and women with the highest adiposity levels and sarcopenia (approximately 6% of the study population) had the greatest risk.
The researchers acknowledged they could not conclusively rule out that sarcopenia may simply be a marker of more aggressive cancer or other factors that could potentially increase the risk of dying.
Although she called it "a valid concern," Dr. Caan pointed to findings in this study that argue against the idea that sarcopenia is simply a byproduct of a more aggressive cancer.
For example, she explained, the extent of the link between sarcopenia and worse survival was the same regardless of whether the women had stage 2 or more-aggressive stage 3 breast cancer. And the increased mortality risk was very similar even when the researchers excluded women who had died within 1 year of their diagnosis, meaning that their cancer was highly aggressive.
The exact relationship between low muscle mass and cancer mortality is "complicated," Dr. Williams said. In other studies, for example, women with metastatic breast cancer who had sarcopenia were much more likely to have severe chemotherapy-related side effects, hospitalizations, and treatment interruptions—all of which can influence how long a patient lives.
"Ultimately, nothing is simple," Dr. Williams said. It's "definitely possible" that the link between sarcopenia and mortality "is a consequence of the biology of the cancer," he continued. "But it's not going to be the full story."
Body Composition and Cancer Care
Dr. Caan said she’s hopeful that muscle mass measurements will begin to be incorporated into standard abdominal CT scan reports. Programs are now available, she added, that can easily capture that information from standard CT scans.
Once information on muscle mass is readily available to clinicians, there are still other important questions to answer, said Dr. Elena, who organized a 2017 NCI-sponsored conference on sarcopenia and cancer.
They include, for example, determining precise muscle mass cutoff levels that put patients at increased mortality risk, she said.
Beyond that, Dr. Williams said, is testing whether information on muscle mass can help improve treatment decisions, such as chemotherapy dose, which is determined based on a patient’s body surface area.
Body surface area is “a crude measure,” he continued. “It’s more than 100 years old.” Using CT scans to differentiate adiposity and muscle mass may eventually “help to inform dosing decisions,” he said.
Drs. Bandera and John said the new findings provide “an important reminder” of incorporating physical activity into the treatment process, “with the goal of not just reducing adiposity, but maintaining and increasing muscle mass.”






















.png)











No hay comentarios:
Publicar un comentario