Vaccine Research: New Tactics for Tackling HIV
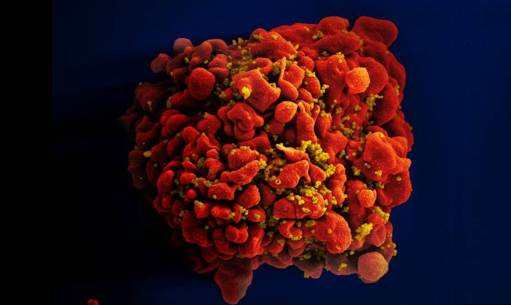
Caption: Scanning electron micrograph of an HIV-infected immune cell.
Credit: National Institute of Allergy and Infectious Diseases, NIH
Credit: National Institute of Allergy and Infectious Diseases, NIH
For many of the viruses that make people sick—think measles, smallpox, or polio—vaccines that deliver weakened or killed virus encourage the immune system to produce antibodies that afford near complete protection in the event of an exposure. But that simple and straightforward approach doesn’t work in the case of human immunodeficiency virus (HIV), the virus that causes AIDS. In part, that’s because our immune system is poorly equipped to recognize HIV and mount an attack against the infection. To make matters worse, HIV has a habit of quickly mutating as it multiplies.That means, in order for an HIV vaccine to be effective, it must induce antibodies capable of fighting against a wide range of HIV strains. For all these reasons, the three decades of effort to develop an HIV vaccine have turned out to be enormously challenging and frustrating.
But now I’m pleased to report that NIH-funded scientists have taken some encouraging strides down this path. In two papers published in Science [1, 2] and one in Cell [3], researchers presented results of animal studies that support what most vaccine experts have come to suspect: the immune system is in fact capable of producing the kind of antibodies that should be protective against HIV, but it takes more than one step to get there. In effect, a successful vaccine strategy has to “take the immune system to school,” and it requires more than one lesson to pass the final exam. Specifically, what’s needed seems to be a series of shots—each consisting of a different engineered protein designed to push the immune system, step by step, toward the production of protective antibodies that will work against virtually all HIV strains.
The new work builds upon basic research discoveries made over the last decade showing that some people infected with HIV eventually do develop a strong immune response that is characterized by broadly neutralizing antibodies (bnAbs) [4,5]. Unfortunately, this response appears only in a minority of people infected with HIV, after years of attack and counterattack between the virus and those individuals’ immune systems. Since those discoveries, vaccine researchers have been busy trying to figure out how to mimic this natural effect in a swifter and more reliable manner that would enable uninfected people to produce bnAbs that could ward off HIV infection.
What makes bnAbs special are their unusual features, which allow them to bind to certain parts of spiky proteins found on the surface, or envelope, of HIV. Unlike many other parts of HIV, these binding sites are “conserved”—which means they don’t change frequently. Researchers regard conserved areas of a virus as ideal targets for the development of vaccines that provide broad, long-lasting protection.
However, a major challenge for HIV vaccine development is that the human genome doesn’t directly code for bnAbs with the ability to bind the virus at its most conserved—and, consequently, most vulnerable—locations. Rather, the development of such bnAbs hinges upon the ability of the antibody genes of certain B cells (a type of white blood cell involved in immune response) to go through a series of DNA rearrangements and mutations, producing precursor proteins that graduallyadapt and change over time into bnAbs capable of neutralizing HIV in its many forms.
In one of the new studies, a team led by David Nemazee, William Schief, and Dennis Burton at The Scripps Institute, La Jolla, CA, reported that it may be possible to optimize bnAb production with a protein nanoparticle specifically engineered to activate the B cells that produce bnAb precursors. In experiments involving a line of mice genetically modified to produce human-like antibodies, the researchers found immunization with an engineered HIV envelope protein, called eOD-GT8 60mer, spurred production of antibodies with some—but not all—of the traits necessary to recognize and block HIV infection. This finding suggests that eOD-GT8 60mer or a similar engineered protein may be a good candidate to serve as the first in a series of immunizations against HIV.
In the second study, a team led by John P. Moore and Rogier Sanders of Weill Medical College of Cornell University, New York, tested the powers of a protein engineered to mimic a highly conserved region of HIV’s envelope proteins.Using rabbit and macaque models, the researchers showed that this protein does elicit an immune response against HIV. Like the protein used in the first study, it did not generate the full neutralizing coverage needed to provide effective protection against a wide range of HIV strains. Still, these findings indicate that one or more proteins designed to mimic this highly conserved portion of HIV should be considered for inclusion in sequential approaches to HIV immunization.
Last but certainly not least, a team led by Schief and Michel Nussenzweig at The Rockefeller University, New York, published a paper that pulls together both new pieces of the HIV vaccine puzzle. Using a different strain of mice, these researchers confirmed that the eOD-GT8 60mer protein does indeed activate the right kind of B cells to get an immune response going. Their experiments in another strain of mice genetically modified to represent a later stage of infection also confirmed that in order to keep the immune response rolling toward truly effective HIV protection, other proteins engineered to mimic HIV envelope proteins will likely be needed. Taken together, these findings provide much-needed, experimental support for the notion that the best bet for an effective HIV vaccine may lie in a strategic sequence of immunizations, each guiding the immune system towards the production of bnAbs.
With about 50,000 Americans and more than 2 million people worldwide becoming newly infected with HIV every year [6], it’s clear that the quest for effective HIV vaccines and treatments has to be a top research priority. There’s a lot of work that still must be done before we can test this sequential HIV vaccine approach in humans, but—as these three new studies show—it looks like science is on a promising new track.
References:
[1] Priming a broadly neutralizing antibody response to HIV-1 using a germline- targeting immunogen. Jardine JG, Ota T, Sok D, Pauthner M, Kulp DW, Kalyuzhniy O, Skog PD, Thinnes TC, Bhullar D, Briney B, Menis S, Jones M, Kubitz M, Spencer S, Adachi Y, Burton DR, Schief WR, Nemazee D. Science. 2015 Jun 18. [Epub ahead of print]
[2] HIV-1 neutralizing antibodies induced by native-like envelope trimers. Sanders RW, van Gils MJ, Derking R, Sok D, Ketas TJ, Burger JA, Ozorowski G, Cupo A, Simonich C, Goo L, Arendt H, Kim HJ, Lee JH, Pugach P, Williams M, Debnath G, Moldt B, van Breemen MJ, Isik G, Medina-Ramírez M, Back JW, Koff WC, Julien JP, Rakasz EG, Seaman MS, Guttman M, Lee KK, Klasse PJ, LaBranche C, Schief WR, Wilson IA, Overbaugh J, Burton DR, Ward AB, Montefiori DC, Dean H, Moore JP. Science. 2015 Jun 18. [Epub ahead of print]
[3] Immunization for HIV-1 broadly neutralizing antibodies in human Ig knockin mice. Dosenovic P, von Boehmer L, Escolano A, Jardine J, Freund NT, Gitlin AD, McGuire AT, Kulp DW, Oliveira T, Scharf L, Pietzsch J, Gray MD, Cupo A, van Gils MJ, Yao KH, Liu C, Gazumyan A, Seaman MS, Björkman PJ, Sanders RW, Moore JP, Stamatatos L, Schief WR, Nussenzweig MC. Cell. 2015 Jun 18;161(7):1505-15.
[4] Broadly neutralizing antibodies and the search for an HIV-1 vaccine: the end of the beginning. Kwong PD, Mascola JR, Nabel GJ. Nat Rev Immunol. 2013 Sep;13(9):693-701.
[5] Broadly neutralizing antibodies and the development of vaccines. Haynes BF, Bradley T. JAMA. 2015 Jun 23-30;(24):2419-2420.
[6] HIV/AIDS: Basic Statistics. Centers for Disease Control and Prevention. May 11, 2015.
Links:
HIV Vaccine Research (National Institute of Allergy and Infectious Diseases/NIH)
Center for HIV/AIDS Vaccine Immunology & Immunogen Discovery (The Scripps Institute, LaJolla, CA)
Michel Nussenzweig (The Rockefeller University, New York)
John P. Moore (Weill Cornell Medical College, New York)
NIH Support: National Institute of Allergy and Infectious Diseases; National Center for Advancing Translational Sciences





















.png)












No hay comentarios:
Publicar un comentario