
FDA Approves Blood Tests That Can Help Guide Cancer Treatment
, by NCI Staff
The Food and Drug Administration (FDA) has approved two blood tests, known as liquid biopsies, that can help guide treatment decisions for people with cancer. The tests, Guardant360 CDx and FoundationOne Liquid CDx, are made by different companies and were approved separately.
Doctors have traditionally based treatment decisions on features like the organ in which the cancer started growing, whether the cancer has spread, and whether the patient has other health conditions. Now they often use another feature to guide treatment: genetic changes in the tumor.
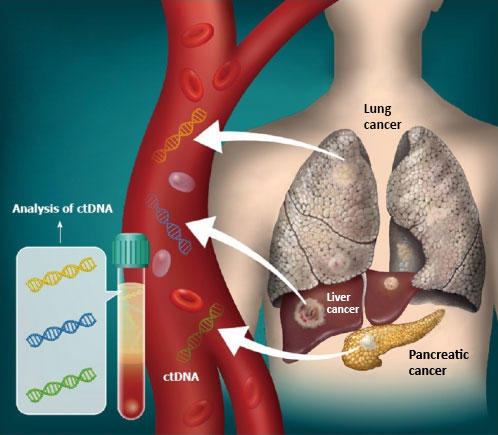
Certain therapies, called targeted therapies and immunotherapies, work best against tumors that have specific genetic changes. The newly approved tests identify genetic changes, including mutations, by scanning DNA that tumors have shed into the blood.
Doctors can then use that information to determine if there is a targeted therapy or immunotherapy that is likely to work for the patient. Analyzing genetic changes in a patient’s cancer is called tumor profiling, genomic profiling, or tumor sequencing.
Both Guardant360 CDx and FoundationOne Liquid CDx are approved for people with any solid cancer (e.g., lung, prostate), but not for those with blood cancers. While FDA has approved other blood tests that check for the presence a single gene mutation in tumor DNA, these are the first approved blood tests that check for multiple cancer-related genetic changes.
Liquid biopsies can sometimes be an alternative to a traditional biopsy, in which a sample of a tumor is removed with a needle or during surgery. They are considered less invasive and quicker than a traditional tissue biopsy.
“Even though the tests have been around for a while, we don’t know how useful they’re really going to be in the clinical setting,” said Ben Ho Park, M.D., Ph.D., of Vanderbilt-Ingram Cancer Center. Many details about how the blood tests may be incorporated into everyday care for people with cancer, including who should get them and whether the cost is covered by private insurance companies, are still being ironed out.
What the FDA’s stamp of approval provides, Dr. Park explained, is validation that the results of a blood-based tumor profiling test can be used to guide the selection of a targeted therapy.
“It’s great that we’ve crossed that hurdle now. It’s great for patients [because] it’s easier to get,” he said.
Companion Diagnostics and General Tumor Profiling
FDA approved Guardant360 CDx on August 7 and FoundationOne Liquid CDx on August 26. The approvals were based on data from hundreds of patients with a range of cancer types. The data showed that the results of both tests agreed with results from other tumor profiling tests that have been proven accurate.
Both tests can be used for two different purposes: as a companion diagnostic test and for general tumor profiling. A test is considered a companion diagnostic if it provides key information about the safe and effective use of a corresponding drug. In this case, the tests determine whether a patient’s tumor has a genetic change that is targeted by a specific drug.
Guardant360 CDx, made by Guardant Health, was approved as a companion diagnostic for osimertinib (Tagrisso), a lung cancer therapy. FoundationOne Liquid CDx, made by Foundation Medicine, was approved as a companion diagnostic for three lung cancer therapies and a prostate cancer therapy. Clinical studies to support additional companion diagnostic labels for both tests are ongoing.
Some of the additional genetic changes covered by the tests are targeted by FDA-approved therapies, but the tests don’t have companion diagnostic designations for those therapies.
For instance, FoundationOne Liquid CDx checks for a genetic feature called microsatellite instability. The drug pembrolizumab (Keytruda) is approved for patients with tumors that have this feature, regardless of where in the body the cancer started growing.
The tests are also approved for general tumor profiling. Guardant360 CDx checks for changes in more than 60 different genes. FoundationOne Liquid CDx, meanwhile, can identify changes in more than 300 genes, as well as other genetic features that make tumors more susceptible to treatment with certain immunotherapies.
If a blood test picks up a genetic change that matches an available treatment, but the test doesn’t have a companion diagnostic label for that drug, “that doesn’t mean it couldn’t work,” Dr. Park explained. “It just means [the company] hasn’t gone through the whole process of getting [their test approved] as a companion diagnostic” for that particular drug, he said.
“The companion diagnostic labels only cover a few genetic changes that match a patient to a particular therapy,” said tumor-profiling expert Ana Robles, Ph.D., of NCI’s Office of Cancer Clinical Proteomics Research. In other words, “the regulations haven’t caught up to the science,” she added.
At some hospitals and cancer centers, groups of doctors with different specialties meet to discuss the patients’ tumor profiling test results. These groups, called molecular tumor boards, take the latest knowledge and research findings into consideration when recommending a treatment, Dr. Park said. He serves on the molecular tumor board at his hospital and studies liquid biopsy tests for breast cancer.
Based on the results of the blood test, an oncologist may end up recommending a targeted therapy for which the test doesn’t have a companion diagnostic approval.
The results of the blood tests could also provide patients with opportunities to join clinical trials. Some studies focus on patients with certain genetic changes present in their cancer, rather than the type of cancer they have.
Who Should Get a Blood Test for Tumor Profiling?
Tumor profiling—either by tissue or blood testing—is recommended for patients with metastatic cancer who don’t have any standard treatment options left or the opportunity to join a clinical trial based on the type of cancer they have, Dr. Park explained.
Although Guardant360 CDx and FoundationOne Liquid CDx are approved for any patient with a solid tumor, there may be specific situations where the tests are best suited, he said.
For instance, there are times when a tissue biopsy may be difficult to do safely because of where the tumor is located, such as in the lung or brain. In that case, it may be better for the person to get a blood test, Dr. Robles said.
Even if the tumor can be reached, some patients aren’t able to get the preferred type of tissue biopsy—what’s called a core biopsy. That could happen if the patient is on blood thinners, doesn’t have enough tumor tissue available, or is too sick to get a core biopsy.
“Again, that might be a situation where we prefer to use a liquid biopsy instead,” Dr. Park said.
But if a patient’s tumor can be easily and safely accessed for a core biopsy, that would be preferred over a liquid biopsy, he noted.
One thing patients might want to consider is whether the cost of the test will be covered by their insurance. Both tests are covered under Medicare. But for private insurance companies, coverage of liquid biopsy tests has varied by the company and the type of test used. In many cases, the cost is only covered if the test was used to check for genetic changes that have companion diagnostic approvals. However, coverage policies for liquid biopsies continue to change.
Are the Tests Sensitive Enough?
When liquid biopsies were first developed, the major question was, “if and when you see [a genetic change] in the blood, can you reliably trust that [it also] exists in the tumor?” said Dr. Robles. Now the consensus is that genetic changes found in the blood accurately represent those present in the tumor, she said.
But there can still be differences between the results of blood- and tissue-based tumor profiling tests, Dr. Robles explained. Those differences may not be because of the blood test’s accuracy, but because of tumor biology, she said. For example, some tumors don’t shed as much DNA into the blood as others do.
Where the tumor is, how big it is, and whether there is more than one tumor also influence how much tumor DNA ends up in the blood, Dr. Park said.
Many times, there is not enough tumor DNA in the patient’s blood for a test to reliably pick up any genetic changes, he explained. “In some ways it’s kind of just luck, whether or not you happen to grab the sample of blood that happens to have enough of that DNA,” he said.
So if a blood-based profiling test doesn’t find any genetic changes, Dr. Park said he would consider that test result to be inconclusive, rather than a negative result.
If that happens, he explained, FDA recommends that the patient get a tissue biopsy to check for genetic changes.





















.png)












No hay comentarios:
Publicar un comentario