
| MMWR Weekly (No. 2) PDF of this issue |
Notes from the Field: Typhoid Fever Outbreak — Harare, Zimbabwe, October 2017–February 2018
Weekly / January 18, 2019 / 68(2);44–45
Hammad S. N’cho, PhD1; Kudzai P.E. Masunda, MBBS2; Innocent Mukeredzi, MPH2; Portia Manangazira, MBBS3; Emmaculate Govore2; Clemence Duri, MBBS2; Rachael D. Aubert, PhD4; Haley Martin4; Elizabeth Gonese, PhD5; Michael Vere, MBchB2; Beth A. Tippett Barr, DrPH5; Shirish Balachandra, MD5; Jonathan Strysko, MD1; William W. Davis, DrPH1; Grace D. Appiah, MD4; Eric Mintz, MD4 (View author affiliations)
View suggested citationOn October 16, 2017, the Harare City Health Department (HCHD) in Zimbabwe identified a suspected typhoid fever (typhoid) case in a resident of Harare’s Mbare suburb. Typhoid is a potentially fatal illness caused by Salmonella enterica serovar Typhi (Typhi). HCHD initiated an investigation and identified a cluster of 17 suspected typhoid cases, defined as the occurrence of fever and at least one of the following symptoms: headache, malaise, abdominal discomfort, vomiting, diarrhea, cough, or constipation. A confirmed case had Typhi isolated from blood, stool, or rectal swab culture (1).
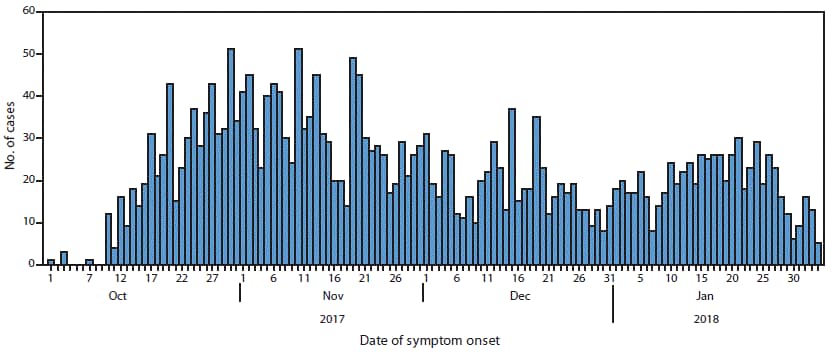
As of February 24, 2018 (the most recent publicly available data), 3,187 suspected and 191 confirmed cases were identified (Figure), with no reported deaths among confirmed cases. Among suspected cases, 1,696 (53%) patients were male, and median age was 17 years (range = 1 month–90 years). In addition to clusters in Mbare, clusters were detected in Harare’s western suburbs, including Kuwadzana, where high rates of ciprofloxacin-resistant Typhi were identified.
Previous typhoid outbreaks in Harare have been associated with municipal water shortages and increased use of contaminated boreholes and shallow wells (2–5). In January 2018, CDC collaborated with HCHD to standardize the collection, analysis, and interpretation of water quality data from wells, boreholes, and municipal taps. HCHD and partners paired this approach with efforts to improve water, sanitation, and hygiene (WASH) through assessing and repairing boreholes (particularly those with in-line chlorinators in affected areas); attending to burst sewers; conducting water sampling of municipal and borehole water; and educating local residents about typhoid. At the request of HCHD, a CDC team also conducted a review of case management and clinical outcomes among suspected typhoid patients admitted to Harare’s designated typhoid treatment center during October 1–December 31, 2017. Among 583 patients admitted with a diagnosis of suspected typhoid, complications occurred in 79 (14%), the most common being acute kidney injury (26), anemia (10), peritonitis (nine), and electrolyte abnormalities (nine). One patient experienced intestinal perforation. Five patients with suspected typhoid died; however, because these cases were not culture-confirmed, they were not reported as typhoid-related deaths. Cultures were processed for 286 (49%) inpatients; 74 (26%) yielded Typhi. Fifteen (33%) of 46 isolates from hospitalized patients were ciprofloxacin-resistant. Complication rates were higher (19%) and median illness duration was longer (9 days) among patients with ciprofloxacin-resistant isolates than among those with nonresistant isolates (9%; 7 days), but the differences were not statistically significant.
CDC laboratorians collaborated with Zimbabwe laboratory staff members to design a reporting protocol for laboratory results and ensure that accurate results of antimicrobial susceptibility testing was included in all reports. The standardized collection and analysis of clinical and laboratory information during an outbreak in which an unusual regional antibiotic resistance pattern featured prominently prompted public health officials to recommend third-generation cephalosporins as first-line treatment for patients residing in areas with high rates of ciprofloxacin resistance (1).
The combination of poor water quality and sanitation and urban overcrowding continues to be a persistent driver of seasonal outbreaks of waterborne diseases in Harare. Although localized WASH interventions, such as those described here, serve to disrupt local transmission, comprehensive measures will be needed to improve the water treatment and delivery system in Harare. One such measure that was informed by the epidemiologic data is a Gavi-funded* vaccination campaign using typhoid conjugate vaccine scheduled for January–February 2019, targeting 350,000 persons; this is the first use of typhoid conjugate vaccine and the first outbreak response vaccination campaign in Africa. The goal of this effort will be to disrupt transmission, thereby providing time for implementation of sustainable and widespread WASH interventions.
Corresponding author: Hammad S. N’cho, HNcho@cdc.gov, 404-718-6775.
1Epidemic Intelligence Service, CDC; 2Harare City Health Department, Harare, Zimbabwe;3Ministry of Health and Child Care, Harare, Zimbabwe; 4Division of Foodborne, Waterborne and Environmental Diseases, National Center for Emerging Zoonotic and Infectious Diseases, CDC; 5Division of Global HIV and TB, Center for Global Health, CDC.
All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
References
- World Health Organization. Guidelines for the management of typhoid fever. Geneva, Switzerland: World Health Organization; 2011. http://apps.who.int/medicinedocs/documents/s20994en/s20994en.pdf
- Davis WW, Chonzi P, Masunda KPE, et al. Notes from the field: typhoid fever outbreak—Harare, Zimbabwe, October 2016–March 2017. MMWR Morb Mortal Wkly Rep 2018;67:342–3.CrossRef PubMed
- CDC. Notes from the field: Salmonella Typhi infections associated with contaminated water—Zimbabwe, October 2011–May 2012. MMWR Morb Mortal Wkly Rep 2012;61:435. PubMed
- Polonsky JA, Martínez-Pino I, Nackers F, et al. Descriptive epidemiology of typhoid fever during an epidemic in Harare, Zimbabwe, 2012. PLoS One 2014;9:. CrossRef PubMed
- Muti M, Gombe N, Tshimanga M, et al. Typhoid outbreak investigation in Dzivaresekwa, suburb of Harare City, Zimbabwe, 2011. Pan Afr Med J 2014;18:309. CrossRef PubMed


































No hay comentarios:
Publicar un comentario