
Invisible wounds: understanding PTSD
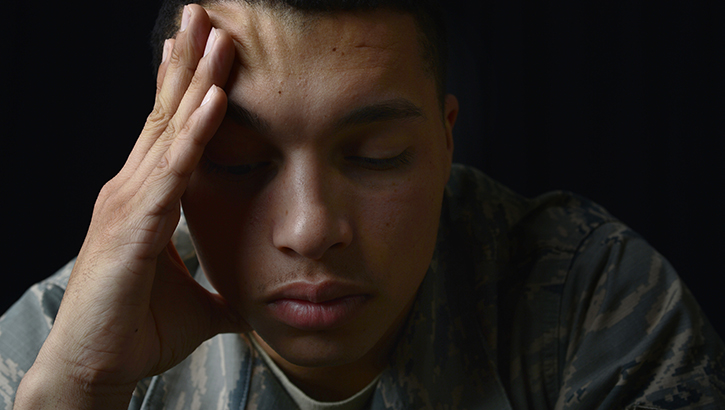
Post-traumatic stress disorder develops in some people after exposure to a traumatic event. It affects approximately 8 million Americans and can interfere with a person’s daily life and impact personal relationships. (U.S. Air Force photo by Senior Airman Christian Clausen/Released)
In the United States, 60% of men and half of all women experience at least one traumatic event in their lives, according to the Department of Veterans Affairs' National Center for PTSD. Roughly 8 million adults live with post-traumatic stress disorder.
Trauma exposure itself doesn’t mean everyone will experience PTSD. “We know that a number of variables put people at risk: prior trauma history, lack of social support, suffering an injury as a result of the trauma, and preexisting mental health issues,” said Holly O’Reilly, a clinical psychologist. The effects of trauma also accrue over time, she added, “So repeated trauma exposure will increase the likelihood of developing post-traumatic symptoms.”
PTSD is a mental health condition that some people develop following exposure to a traumatic event, said O’Reilly, who works at the Psychological Health Center of Excellence, a division of the Defense Health Agency Research and Development Directorate. Although anxiety and depression can overlap with PTSD symptoms, the conditions are different. Anxiety is a pattern of worrying or being fearful of something that could happen while depression refers to a depressed mood for two weeks or more, explained O’Reilly. “Individuals with symptoms of PTSD continue to be anxious as a result of a prior trauma experience or exposure,” she said.
An official diagnosis of PTSD requires exposure to a traumatic event and symptoms from four different categories. They include reliving trauma through intrusive memories; avoidance of any reminders of trauma; persistent negative thoughts and emotions associated with the trauma; and hyperarousal, which is consistently feeling “on edge,” particularly in response to reminders of the trauma. People may be easily startled, feel irritable, or have difficulty falling asleep.
PTSD can interfere with a person’s daily life and impact personal relationships. “Individuals who have symptoms of PTSD may demonstrate difficulty completing everyday tasks, experience persistent anxiety, or have upsetting reminders of previous traumatic events,” said O’Reilly.
As people practice social distancing, social isolation may contribute to PTSD symptoms, she cautioned. If a person used social activity to avoid intense emotions, the loss of social activity could lead to thinking about past trauma and a worsening of symptoms.
“Research has shown that PTSD can be treated successfully via evidence-based psychotherapy,” she said. “The best way for individuals to fully recover is to fully participate in evidence-based psychotherapy, allowing them to process their response to the trauma and learn skills to move forward.”
A common misconception is that a diagnosis of PTSD will negatively impact a person’s career, but without treatment, symptoms will persist and may even worsen. PTSD treatments work and people can fully recover, said O’Reilly. Even years after the initial trauma, people can still benefit from treatment, but the sooner a person seeks therapy, the better. Many types of evidence-based PTSD treatment usually take two to three months to complete and occur in weekly individual sessions. O’Reilly encourages practicing new therapy skills outside of the sessions.
PTSD can result in changes to changes in the brain, but it may not be permanent, said Dr. Robert Ursano, director of the Uniformed Services University of the Health Sciences’ Center for the Study of Traumatic Stress, who spoke recently at a PTSD roundtable. “We know specifically three primary and several other areas in the brain but principally the prefrontal cortex, the hippocampus and the medulla show alterations in those with PTSD versus that those who don't,” he said. “We also have data that showed that after treatment the brain can change back again.” PTSD is a highly treatable disorder with effective medications and psychotherapies, he added.
“If you or someone you care about has symptoms of PTSD and they cause distress or interfere with daily activities, you should seek help from your local behavioral health clinic,” said O’Reilly, adding all military hospitals and clinics have PTSD experts available. “You may also connect through Military One Source, or the inTransition program,” she added. Resources on PTSD treatment are available on the Psychological Health Center of Excellence website.
MHS mental health experts shed light on PTSD
Article
6/22/2020

Media roundtable event recognizes PTSD Awareness Month
The Language of Anger and Depression Among Patients with Concussions
Article
6/4/2020

Soldiers often do not overtly express their feelings of depression.
'Home sweet home' leaves a sour taste for some quarantine-weary
Article
5/28/2020

Mental health professionals offer tips on managing during uncertain times
Using mobile mental health apps to cope during social isolation
Article
5/22/2020

Learn how your smartphone can serve as a lifeline
Military chaplains emphasize spiritual health during COVID-19 pandemic
Article
5/19/2020

In a time of great fear, spiritual health remains an important domain of Total Force Fitness.
Army veterinarians post FAQ for pet owners to Army Public Health Center COVID-19 website
Article
4/30/2020

Studies are underway to investigate human to animal transmission in multiple animal species.
inTransition Teams Up with the Veterans Crisis Line to Support Service Members in Crisis
Article
4/10/2020

In response to an increased volume of calls to the Veterans Crisis Line (VCL) since the outbreak of the novel coronavirus (COVID-19), inTransition is partnering with the VCL to coordinate certain types of care for active duty service members.
Coping with the stress of social distancing
Article
3/31/2020

How to navigate the COVID-19 outbreak
McCaffery offers MHS view with Blue Star Families panel
Article
2/28/2020
The Honorable Thomas McCaffery participated in the Blue Star Families panel to discuss MHS transformation for families
DHA PM 6025-01: Primary Care Behavioral Health (PCBH) Standards
Policy
This Defense Health Agency-Procedures Manual (DHA-PM), based on the authority of References (a) and (b), and in accordance with the guidance of References (c) through (i), establishes the Defense Health Agency’s (DHA) procedures to establish required standards for: a. Military Medical Treatment Facilities (MTFs) and primary care clinics for adult, child and adolescent, health behavior, behavioral medicine, and behavioral health services in primary care. b. Behavioral Health Consultants (BHCs). c. Behavioral Health Care Facilitators (BHCFs). d. External Behavioral Health Consultants (EBHCs). e. Primary Care Clinic Leaders.
- Identification #: 6025.01
- Date: 1/10/2020
- Type: Memorandums
- Topics: Mental Wellness | Mental Health Care
Mental Health Professionals
Congressional Testimony
11/26/2019
S. 3129, SAC Report for FY 2019, 115-290, Pg. 211
Positive attitude, social support may promote TBI/PTSD resilience
Article
7/23/2019

Psychological experiences prior to an injury may play a role in recovery
Warm Handoff for Transitioning Servicemembers Suffering from PTSD and TBI
Congressional Testimony
7/8/2019
S. 2987, SASC Report for FY 2019, 115-262, Pg. 203-204
New clinical recommendations on cognitive rehabilitation for TBI released
Article
6/24/2019

Cognitive rehabilitation focuses on improving thinking and communication skills
Practicing yoga to stimulate the mind, body, spirit
Article
6/21/2019

Programs at Walter Reed incorporate yoga basics to promote healing





















.png)












No hay comentarios:
Publicar un comentario