Considerations for Wearing Cloth Face Coverings
Help Slow the Spread of COVID-19
On This Page
- CDC recommends that people wear cloth face coverings in public settings and when around people outside of their household, especially when other social distancing measures are difficult to maintain.
- Cloth face coverings may help prevent people who have COVID-19 from spreading the virus to others.
- Cloth face coverings are most likely to reduce the spread of COVID-19 when they are widely used by people in public settings.
- Cloth face coverings should NOT be worn by children under the age of 2 or anyone who has trouble breathing, is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.
Evidence for Effectiveness of Cloth Face Coverings
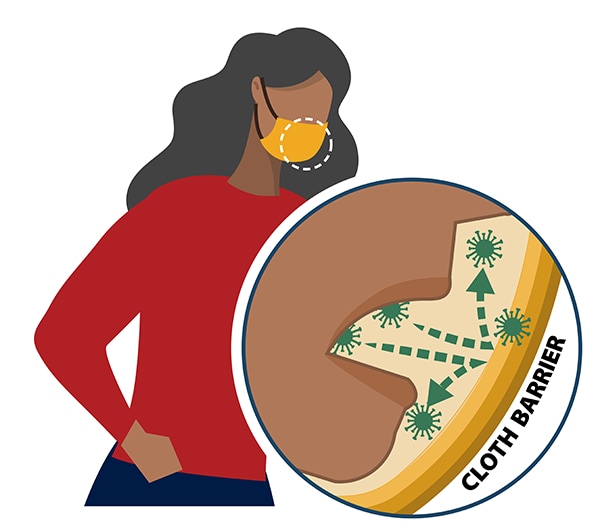
Cloth face coverings are recommended as a simple barrier to help prevent respiratory droplets from traveling into the air and onto other people when the person wearing the cloth face covering coughs, sneezes, talks, or raises their voice. This is called source control. This recommendation is based on what we know about the role respiratory droplets play in the spread of the virus that causes COVID-19, paired with emerging evidence from clinical and laboratory studies that shows cloth face coverings reduce the spray of droplets when worn over the nose and mouth. COVID-19 spreads mainly among people who are in close contact with one another (within about 6 feet), so the use of cloth face coverings is particularly important in settings where people are close to each other or where social distancing is difficult to maintain.
Who Should Wear A Cloth Face Covering?
General public
- CDC recommends all people 2 years of age and older wear a cloth face covering in public settings and when around people outside of their household, especially when other social distancing measures are difficult to maintain.
- COVID-19 can be spread by people who do not have symptoms and do not know that they are infected. That’s why it’s important for everyone to wear cloth face coverings in public settings and practice social distancing (staying at least 6 feet away from other people).
- While cloth face coverings are strongly encouraged to reduce the spread of COVID-19, CDC recognizes there are specific instances when wearing a cloth face covering may not be feasible. In these instances, adaptations and alternatives should be considered whenever possible (see below for examples).
People who know or think they might have COVID-19
- If you are sick with COVID-19 or think you might have COVID-19, do not visit public areas. Stay home except to get medical care. As much as possible stay in a specific room and away from other people and pets in your home. If you need to be around other people or animals, wear a cloth face covering (including in your home).
- The cloth face covering helps prevent a person who is sick from spreading the virus to others. It helps keep respiratory droplets contained and from reaching other people.
Caregivers of people with COVID-19
- Those caring for someone who is sick with COVID-19 at home or in a non-healthcare setting may also wear a cloth face covering. However, the protective effects—how well the cloth face covering protects healthy people from breathing in the virus—are unknown. To prevent getting sick, caregivers should also continue to practice everyday preventive actions: avoid close contact as much as possible, clean hands often; avoid touching your eyes, nose, and mouth with unwashed hands; and frequently clean and disinfect surfaces.
Who Should Not Wear a Cloth Face Covering
Cloth face coverings should not be worn by:
- Children younger than 2 years old
- Anyone who has trouble breathing
- Anyone who is unconscious, incapacitated, or otherwise unable to remove the cloth face covering without assistance
Feasibility and Adaptations
CDC recognizes that wearing cloth face coverings may not be possible in every situation or for some people. In some situations, wearing a cloth face covering may exacerbate a physical or mental health condition, lead to a medical emergency, or introduce significant safety concerns. Adaptations and alternatives should be considered whenever possible to increase the feasibility of wearing a cloth face covering or to reduce the risk of COVID-19 spreading if it is not possible to wear one.
For example,
- Individuals who are deaf or hard of hearing—or those who care for or interact with a person who is hearing impaired—may be unable to wear cloth face coverings if they rely on lipreading to communicate. In this situation, consider using a clear face covering. If a clear face covering isn’t available, consider whether you can use written communication, use closed captioning, or decrease background noise to make communication possible while wearing a cloth face covering that blocks your lips.
- Some individuals with developmental disabilities, sensory integration concerns or tactile sensitivities, certain mental health conditions, or limited cognitive ability may have a negative reaction to wearing a cloth face covering. These individuals may consult with their healthcare provider as part of the decision to wear a cloth face covering.
- Younger children (e.g., preschool or early elementary aged) may be unable to wear a cloth face covering properly, particularly for an extended period of time. Wearing of cloth face coverings may be prioritized at times when it is difficult to maintain a distance of 6 feet from others (e.g., during carpool drop off or pick up, or when standing in line at school). Ensuring proper cloth face covering size and fit and providing children with frequent reminders and education on the importance and proper wear of cloth face coverings may help address these issues.
- Individuals should not wear cloth face coverings while engaged in activities that may cause the cloth face covering to become wet, like when swimming at the beach or pool. A wet cloth face covering may make it difficult to breathe. For activities like swimming, it is particularly important to maintain physical distance from others when in the water.
- Individuals who are engaged in high intensity activities, like running, may not be able to wear a cloth face covering if it causes difficulty breathing. If unable to wear a cloth face covering, consider conducting the activity in a location with greater ventilation and air exchange (for instance, outdoors versus indoors) and where it is possible to maintain physical distance from others.
- Individuals who work in a setting where cloth face coverings may increase the risk of heat-related illness or cause safety concerns due to introduction of a hazard (for instance, straps getting caught in machinery) may consult with an occupational safety and health professional to determine the appropriate face covering for their setting. Outdoor workers may prioritize use of cloth face coverings when in close contact with other people, like during group travel or shift meetings, and remove face coverings when social distancing is possible. Find more information here and below.
Cloth face coverings are a critical preventive measure and are most essential in times when social distancing is difficult. If cloth face coverings cannot be used, make sure to take other measures to reduce the risk of COVID-19 spread, including social distancing, frequent hand washing, and cleaning and disinfecting frequently touched surfaces.
Face Shields
It is not known if face shields provide any benefit as source control to protect others from the spray of respiratory particles. CDC does not recommend use of face shields for normal everyday activities or as a substitute for cloth face coverings. Some people may choose to use a face shield when sustained close contact with other people is expected. If face shields are used without a mask, they should wrap around the sides of the wearer’s face and extend to below the chin. Disposable face shields should only be worn for a single use. Reusable face shields should be cleaned and disinfected after each use. Plastic face shields for newborns and infants are NOT recommended.
Surgical Masks
Cloth face coverings are not surgical masks or respirators. Currently, those are critical supplies that should continue to be reserved for healthcare workers and other medical first responders, as recommended by current CDC guidance. Cloth face coverings also are not appropriate substitutes for them in workplaces where masks or respirators are recommended or required and available.
Recent Studies:
- Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. The New England journal of medicine. 2020;382(10):970-971. PMID: 32003551
- Zou L, Ruan F, Huang M, et al. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. The New England journal of medicine. 2020;382(12):1177-1179. PMID: 32074444
- Pan X, Chen D, Xia Y, et al. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. The Lancet Infectious diseases. 2020. PMID: 32087116
- Bai Y, Yao L, Wei T, et al. Presumed Asymptomatic Carrier Transmission of COVID-19. Jama. 2020. PMID: 32083643
- Kimball A HK, Arons M, et al. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility — King County, Washington, March 2020. MMWR Morbidity and mortality weekly report. 2020; ePub: 27 March 2020. PMID: 32240128
- Wei WE LZ, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;ePub: 1 April 2020. PMID: 32271722
- Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science (New York, NY). 2020. PMID: 32179701
- Furukawa NW, Brooks JT, Sobel J. Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic [published online ahead of print, 2020 May 4]. Emerg Infect Dis. 2020;26(7):10.3201/eid2607.201595. Link
- Oran DP, Topol Prevalence of Asymptomatic SARS-CoV-2 Infection: A Narrative Review [published online ahead of print, 2020 Jun 3]. Ann Intern Med. 2020;M20-3012. PMID: 32491919
- National Academies of Sciences, Engineering, and Medicine. 2020. Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic (April 1, 2020). Washington, DC: The National Academies Press. https://doi.org/10.17226/25769.
- Schwartz KL, Murti M, Finkelstein M, et al. Lack of COVID-19 transmission on an international flight. CMAJ. 2020;192(15):E410. PMID: 32392504
- Anfinrud P, Stadnytskyi V, Bax CE, Bax A. Visualizing Speech-Generated Oral Fluid Droplets with Laser Light Scattering. N Engl J Med. 2020 Apr 15. doi:10.1056/NEJMc2007800. PMID: 32294341
- Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013;7(4):413-8. PMID: 24229526
- Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano. 2020 Apr 24. PMID: 32329337
- Aydin O, Emon B, Saif MTA. Performance of fabrics for home-made masks against spread of respiratory infection through droplets: a quantitative mechanistic study. medRxiv preprint doi: https://doi.org/10.1101/2020.04.19.20071779, posted April 24, 2020.
- Ma QX, Shan H, Zhang HL, Li GM, Yang RM, Chen JM. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020. PMID: 32232986


































No hay comentarios:
Publicar un comentario