Chronic Diseases and Cognitive Decline — A Public Health Issue

People are living longer and by 2030 about one in five Americans will be aged 65 years and older.1 Although increased longevity brings with it many benefits, not all adults necessarily experience good health and well-being as they age.2–4 Older adults are at a significant risk of having multiple chronic diseases, also known as comorbidities or multi-morbidities, and associated functional impairment.5–8 Functional impairment refers to limitations in the ability to carry out day-to-day household activities and chores or experiencing interference in engaging in activities outside of the home.3,10 As they continue to age, many older adults live with a growing number of complex health issues that adversely affect their day-to-day functioning and overall quality of life.9 For some people and groups of older adults, these concerns are further compounded by the presence of memory issues.
Subjective cognitive decline (SCD) is the self-reported experience of worsening or more frequent confusion or memory loss within the past year.2,3 It is a form of cognitive impairment and one of the earliest noticeable symptoms of more severe memory disorders such as Alzheimer’s disease and related dementias.3,11
SCD can have detrimental implications for living with and managing chronic diseases, or performing everyday activities like cooking or cleaning.3 When cognition is impaired, it can have a profound impact on an individual’s overall health and well-being.
Additionally, people with chronic conditions, such as coronary heart disease, stroke, diabetes, cancer, chronic obstructive pulmonary disease (COPD), arthritis, and kidney disease, who also
have Alzheimer’s or other dementias have higher use and costs of health care services than people with these chronic conditions who do not have Alzheimer’s or other dementias.11
have Alzheimer’s or other dementias have higher use and costs of health care services than people with these chronic conditions who do not have Alzheimer’s or other dementias.11
This Chronic Diseases and Cognitive Decline – A Public Health Issue brief is the fourth of a series of topic-specific documents focusing on public health issues related to older adults. The series of briefs provide public health professionals with recent data on health and age-related conditions, the importance of brain health, and the management of chronic conditions to help identify needs and mitigate the future health burden associated with a growing proportion of older adults.
SCD can have detrimental implications for living with and managing chronic diseases, or performing everyday activities like cooking or cleaning.3 When cognition is impaired, it can have a profound impact on an individual’s overall health and well-being.

This brief examines the following topics:
- Demographic characteristics of those who reported chronic diseases and SCD
- Types of chronic diseases and SCD
- Number of co-morbid chronic diseases and SCD
- Discussing chronic diseases and SCD
This brief presents the characteristics of middle-aged and older adults, those aged 45 years and older, who reported SCD and one or more chronic diseases. Data presented in this brief were collected from community-dwelling adults in 2015–2017 through the Behavioral Risk Factor Surveillance System (BRFSS). Questions related to SCD were administered as part of the BRFSS in 49 states, the District of Columbia (D.C.) and Puerto Rico.2,5 For states administering the module during multiple years, the most recent data were used for this brief. Additional data reports can be generated and viewed through the CDC’s Alzheimer’s Disease and Healthy Aging Data Portal.2
These data were examined by age group, sex, race/ethnicity, chronic disease status, SCD status, and other demographic characteristics. Subjective cognitive decline infographics can be viewed and downloaded through the CDC Alzheimer’s Disease and Healthy Aging Website .2
Demographic Characteristics of Adults by Subjective Cognitive Decline and Chronic Diseasea Status
| With Subjective Cognitive Decline | Without Subjective Cognitive Decline | |||
|---|---|---|---|---|
| Age Group | No Chronic Disease (%) | At Least One Chronic Disease (%) | No Chronic Disease (%) | At Least One Chronic Disease (%) |
| 45-64 years | 22.6 | 77.4 | 52.9 | 47.1 |
| 65+ years | 13.7 | 86.3 | 26.5 | 73.5 |
| Sex | ||||
| Female | 16.2 | 83.8 | 40.1 | 59.9 |
| Male | 22.2 | 77.8 | 46.4 | 53.6 |
| Race and Ethnicity | ||||
| Non-Hispanic white | 18.5 | 81.5 | 42.2 | 57.8 |
| Non-Hispanic black | 13.6 | 86.4 | 39.9 | 60.1 |
| Non-Hispanic American Indian and Alaskan Native | 11.6 | 88.4 | 32.6 | 67.4 |
| Non-Hispanic Asian and Pacific Islander | 50.4 | 49.6 | 50.2 | 49.8 |
| Non-Hispanic of other or multiple races | 12.3 | 87.7 | 35.7 | 64.3 |
| Hispanic, any race | 23.8 | 76.2 | 50.6 | 49.4 |
| Highest Level of Education | ||||
| Did not graduate from high school | 17.3 | 82.7 | 33.6 | 66.4 |
| Graduated high school | 16.5 | 83.5 | 39.1 | 60.9 |
| Some college or technical school | 17.9 | 82.1 | 42.2 | 57.8 |
| Graduated college or technical school | 27.5 | 72.5 | 51.6 | 48.4 |
| Living Status | ||||
| Lives alone | 15.8 | 84.2 | 34.8 | 65.2 |
| Does not live alone | 20.6 | 79.4 | 45.5 | 54.2 |
Across all demographic characteristics except for non-Hispanic Asian and Pacific Islanders, a higher proportion of those with SCD reported having at least one chronic disease than those without SCD.
Age: The prevalence of having at least one chronic disease was lower among adults aged 45–64 years than those aged 65 years and older.
Sex: Of adults aged 45 years and older with SCD, women had a higher prevalence (83.8%) of having at least one chronic disease compared with men (77.8%).
Race and ethnicity: Across all races, except for non-Hispanic Asians and Pacific Islanders, those with SCD had a higher prevalence of having one or more chronic diseases than those without SCD.
Education: Among both adults with and without SCD, those with at least a college degree have a lower prevalence of having at least one chronic disease compared with those with less than a college degree.
Living status: Among adults with SCD, those who live alone reported a higher prevalence (84.2%) of having at least one chronic disease compared with those who do not live alone (79.4%).
Type of Chronic Disease and Subjective Cognitive Decline Status
| Age 45–64 years | Age 65+ years | |||
|---|---|---|---|---|
| Disease | Without SCD (%) | With SCD (%) | Without SCD (%) | With SCD (%) |
| Arthritis | 29.6 | 60.3 | 49.4 | 63.9 |
| Asthma | 8.5 | 18.5 | 7.8 | 11.8 |
| Caner | 6.8 | 11.6 | 17.5 | 20.7 |
| COPD | 6.2 | 22.1 | 11.2 | 22.0 |
| Coronary Heart Diseaseb | 5.7 | 17.5 | 16.3 | 27.6 |
| Diabetes | 13.4 | 24.0 | 22.3 | 30.2 |
| Kidney Disease | 2.6 | 7.4 | 5.5 | 10.5 |
| Stroke | 2.7 | 11.6 | 6.6 | 15.0 |

Compared with those without SCD, adults aged 45 years and older with SCD were more likely to have coronary heart disease, stroke, diabetes, asthma, COPD, cancer, arthritis, or kidney disease. However, adults aged 65 years and older were more likely to report SCD compared with adults aged 45-64. Some studies have shown that 50% of adults 65 years and older with SCD develop more severe cognitive decline within 7–18 years.(4,11)
Number of Co-morbid Chronic Diseases and Subjective Cognitive Decline Status
The presence of memory loss or confusion can disrupt a person’s ability to live independently, especially in a way that allows them to avoid risks to their future health. Furthermore, memory loss can complicate the management of chronic diseases, particularly for those experiencing multiple co-morbid chronic diseases.
Figure 1: Adults aged 45–64 years by number of co-morbid chronic diseases and subjective cognitive decline status
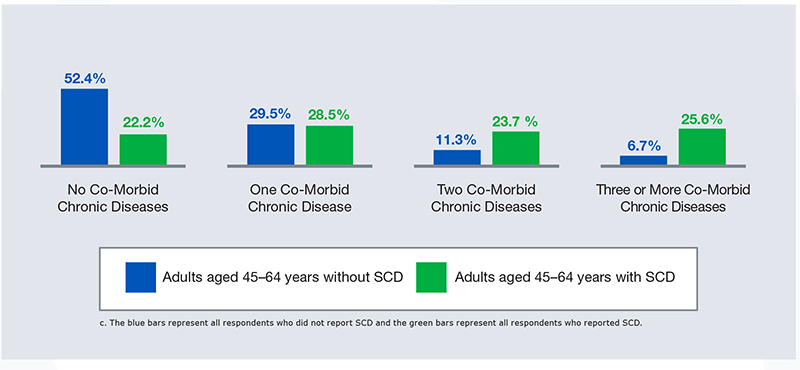
| Adults aged 45-64 years without SCD | Adults aged 45-64 years with SCD | |
|---|---|---|
| No Co-Morbid Chronic Diseases | 52.4 % | 22.2 % |
| One Co-Morbid Chronic Diseases | 29.5 % | 28.5 % |
| Two Co-Morbid Chronic Diseases | 11.3 % | 23.7 % |
| Three or More Co-Morbid Chronic Diseases | 6.7 % | 25.6 % |

Among those with or without SCD, the number of chronic diseases reported varied. A chronic disease was reported with responses by respondents to ever having been told by a provider that they had a previous diagnosis of one of the following eight chronic diseases: asthma, COPD, coronary heart disease, arthritis, stroke, kidney disease, cancer,and diabetes. The prevalence of co-morbid chronic diseases was higher in those with SCD compared to those without. For persons aged 45–64 years, the prevalence of those who reported two or more chronic diseases was higher among those who reported SCD than those without SCD.
Figure 2: Adults aged 65 years and older by number of co-morbid chronic diseases and subjective cognitive decline status
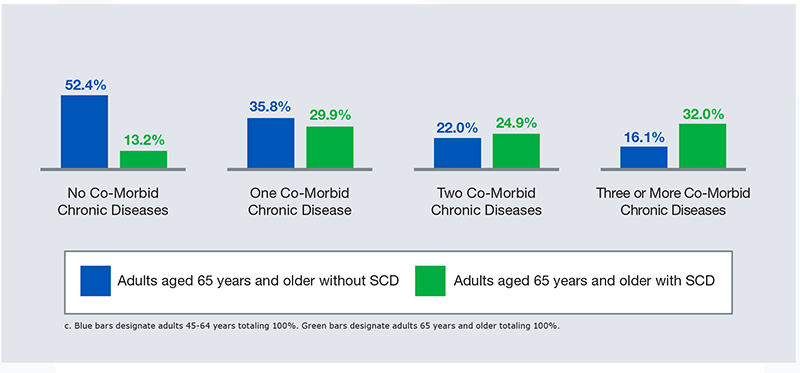
| Adults aged 65 years and older without SCD | Adults aged 65 years and older with SCD | |
|---|---|---|
| No Co-Morbid Chronic Diseases | 52.4 % | 13.2 % |
| One Co-Morbid Chronic Disease | 35.8 % | 29.9 % |
| Two Co-Morbid Chronic Diseases | 22.0 % | 24.9 % |
| Three or More Co-Morbid Chronic Diseases | 16.1 % | 32.0 % |
For persons aged 65 years and older, the prevalence of having one or more chronic diseases was higher than those aged 45–64 years. Among adults aged 65 years and older, the prevalence of those who reported having three or more chronic diseases was higher among those with SCD than those without SCD. Both the prevalence of SCD and chronic diseases increase with age. Poorly managed chronic diseases could lead to further cognitive impairment, adding to the impact of SCD on the patient’s ability tomanage diseases. This may lead to poorer health outcomes, including preventable hospitalizations, or more severe symptoms of memory loss and/or confusion. Among both age groups, adults with SCD were more likely to have one or more chronic diseases compared with those without SCD. About twice as many adults without SCD had no chronic diseases compared with those reporting SCD.
Prevalence of Subjective Cognitive Decline Among Those with Chronic Diseases
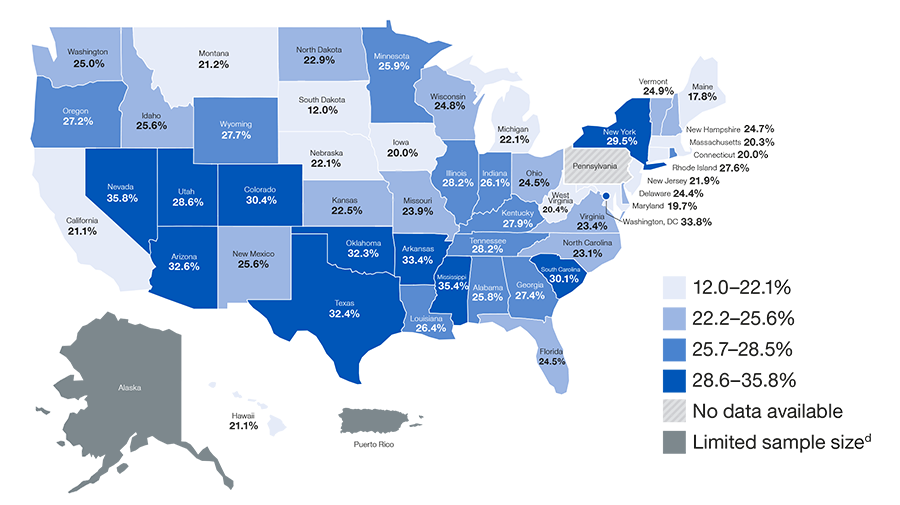
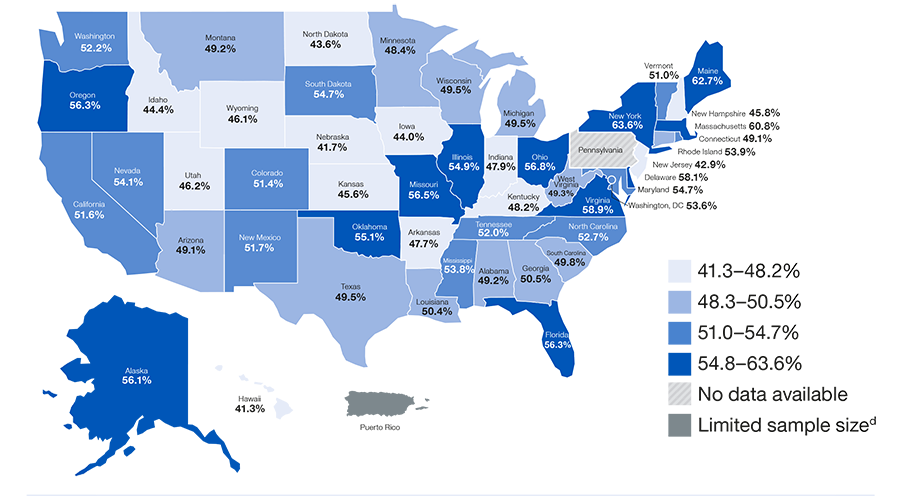
Figure 3: Adults aged 45 years and older with one or more chronic diseases who reported subjective cognitive decline
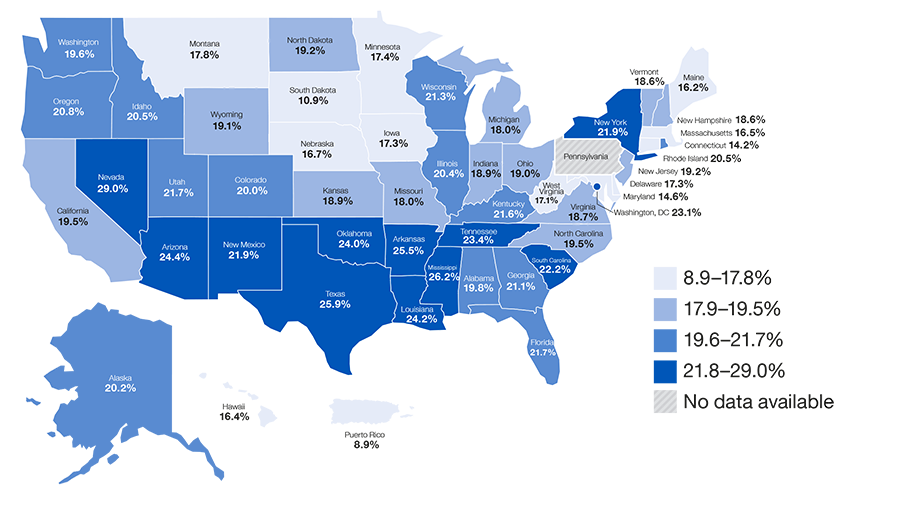
During the past 12 months, have you experienced confusion or memory loss that is happening more often or is getting worse?
• Among adults aged 45 years and older with one or more chronic diseases, 20.4% reported having subjective cognitive decline.
• 20 states, D.C., and Puerto Rico had prevalence of SCD among those with one or more chronic diseases that were higher than 20.4%.
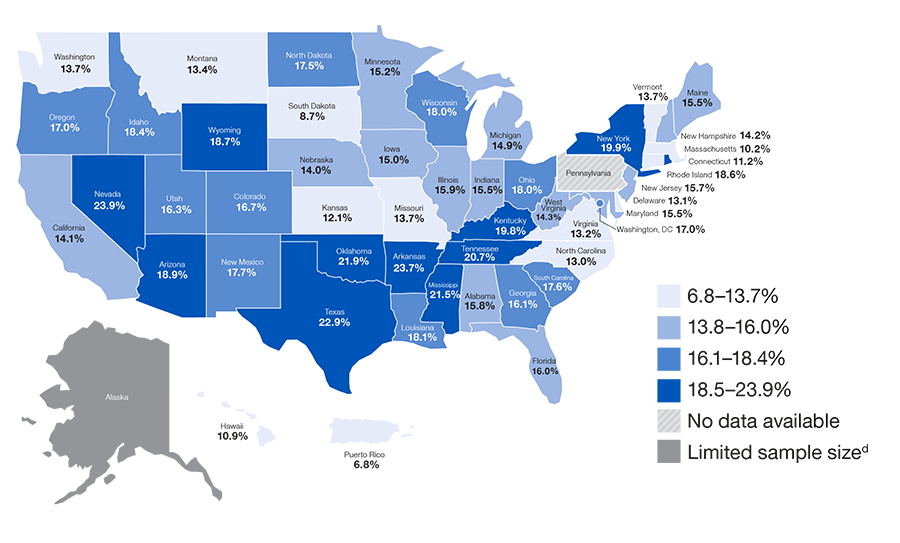
Figure 4: Adults aged 45 years and older with three or more chronic diseases who reported subjective cognitive decline
d. Limited Sample size refers to the low number of telephone participants included in the BRFS study which reduces quality of study results.

Has a doctor, nurse or other health professional EVER told you that you had one of the following: a heart attack, angina or coronary heart disease, stroke, asthma (still have), cancer (skin, other types of cancer), COPD, arthritis, kidney disease, or diabetes?
• About 1 in 4 (25.6%) adults aged 45 years and older with three or more chronic diseases also reported SCD.
• 26 states, D.C., and Puerto Rico had a prevalence of SCD among those with three or more chronic diseases that were higher than 25.6%.
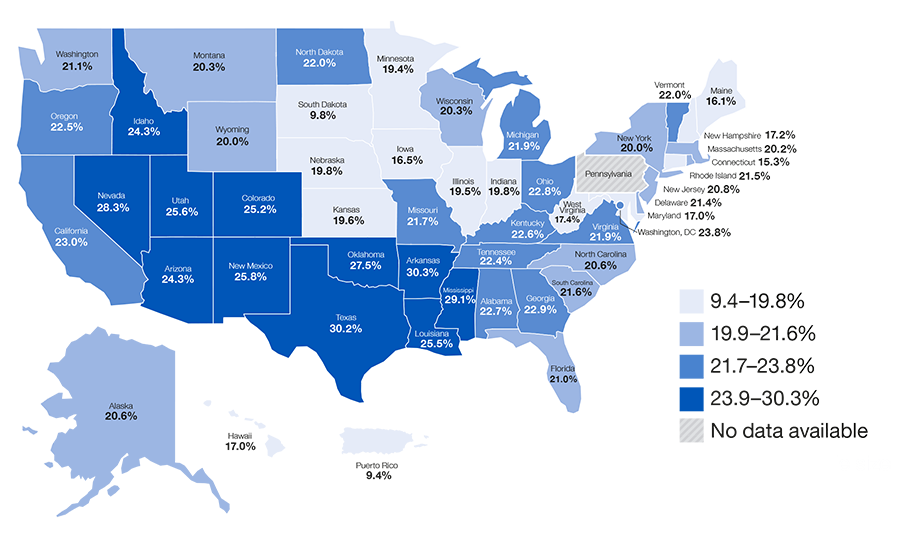
Figure 5: Adults aged 45 years and older with diabetes who reported subjective cognitive decline
d. Limited Sample size refers to the low number of telephone participants included in the BRFSS study which reduces quality of study results.
Has a doctor, nurse or other health professional ever told you that you had diabetes?
Diabetes, both type 1 and type 2, can lead to decreased cognitive function that can impact effective diabetes self-management.12,13,14 Cognitive impairment in areas of learning, memory, and decision-making can increase the need for assistance in self-management, such as the need for help with medication management or scheduling medical appointments.12,13 Adults with diabetes who report SCD have been found to have increased potential for functional difficulties. Functional difficulties are defined as interfering with a person’s ability to engage in activities that they typically perform, like chores, socializing, taking medications, or working outside the home.12,13
• 16.1% of adults aged 45 years and older with diabetes reported having SCD.
Figure 6: Adults aged 45 years and older with coronary heart disease, stroke, or both who reported subjective cognitive decline
a. Respondents were classified as having coronary heart disease (CHD) if they reported having been told by a provider they had CHD, a heart attack (i.e., myocardial infarction), or angina.

Has a doctor, nurse or other health professional ever told you that you had one of the following: a heart attack, angina or coronary heart disease, or a stroke?
Coronary heart disease can lead to decreased cognitive function.15 Intensive blood pressure control may reduce the risk for cognitive decline.17 Cognitive
decline can impact effective chronic disease self management and successful activities of daily living.15-18
decline can impact effective chronic disease self management and successful activities of daily living.15-18
• 22.2% of adults who reported CHD, a stroke, or both reported subjective cognitive decline.
• 27.1% of adults aged 45–64 years who reported CHD, or a stroke, or both reported subjective cognitive decline compared with 18.7% of adults 65 years of age and older.
Discussing Chronic Diseases and Subjective Cognitive Decline
Figure 7: Adults aged 45 years and older with one or more chronic diseases and subjective cognitive decline who reported discussing their subjective cognitive decline with a health care professional
d. Limited Sample size refers to the low number of telephone participants included in the BRFSS study which reduces quality of study results.
Have you or anyone else discussed your confusion or memory loss with a health care professional?
• Although nearly half (48.3%) of adults aged 45 and older with more than one chronic disease and subjective cognitive decline reported discussing their subjective cognitive decline with a health care professional, adults without chronic diseases were less likely to discuss symptoms of SCD with a health care professional.
The disparity between those with and without chronic diseases who discussed symptoms of SCD with a health care professional appears greater among middle-aged than older adults. Among adults aged 45–64, 54.2% of those with at least one chronic disease reported discussing symptoms of SCD with a health care professional while only 30.8% of those with no chronic diseases reported discussing SCD with a health care professional. Among adults aged 65 years and older, 41.0% of those with one or more chronic disease discussed SCD while 32.3% of those with no chronic diseases discussed SCD.
Researchers have found that few adults with SCD discussed their confusion or memory loss with a health care professional.19,20 In fact, the prevalence of cognitive decline identified in community surveys is over twice that reported in medical records of general practitioners.2,3 Opportunities for improvement exist for increased screening, diagnosis, and identification of treatable cause(s).2
Multiple chronic diseases (two or more) have been found to be associated with increased potential for functional difficulties.16 These difficulties can be further exacerbated by the presence of worsening memory. Among adults aged 45 years and older, those with one or more co-morbid chronic diseases reported a higher likelihood of having SCD interfere with their daily lives than those with no chronic diseases. Additional challenges for thosewith one or more chronic diseases include having to give up household activities or chores as a result of SCD, or having SCD interfere with one’s ability to work, volunteer, or engage in social activities outside the home.
Call to Action
Subjective cognitive decline (SCD) is a public health issue. Public health has a role in minimizing its impact. The prevalence of memory loss and chronic diseases increase with age. Improving the management of chronic diseases and accounting for memory concerns in people aged 45 years and older may improve health outcomes. Below are some of the actions that can be taken to improve the health and well-being of persons experiencing chronic diseases and memory loss.
1. Increase awareness about the importance of managing chronic diseases, including diseases associated with coronary heart disease or stroke, among people with subjective cognitive decline (SCD).
- People with SCD are more likely to have multiple co-morbid chronic diseases which can complicate
management.
2. Encourage patients and health care professionals to discuss any memory concerns during routine medical office visits.
- Use Welcome to Medicare and Medicare Annual Wellness Visits to improve management of chronic diseases among older adults and discuss symptoms of SCD.
3. Educate healthcare professionals about the importance of treating co-morbidities and addressing injury risks among patients with memory loss.
4. Raise awareness about the best available evidence on dementia including risk reduction and early
detection.
detection.
5. Emphasize the importance of effective self-management strategies for adults with chronic diseases,
especially among those experiencing memory loss.
especially among those experiencing memory loss.
6. Promote quality tools and information to health care, public health, and social services workers who
deliver care to individuals with multiple chronic conditions and SCD.
deliver care to individuals with multiple chronic conditions and SCD.
7. Facilitate research to fill knowledge gaps about, and interventions and systems to benefit, individuals
with multiple chronic conditions.
with multiple chronic conditions.
Technical Information
The Behavioral Risk Factor Surveillance System (BRFSS) is the nation’s premier system of health-related telephone surveys that collect state data about U.S. residents regarding their health-related risk behaviors, chronic diseases, and use of preventive services. Established in 1984 with 15 states, BRFSS now collects data in all 50 states as well as the District of Columbia and three U.S. territories. BRFSS completes more than 450,000 adult interviews each year, making it the largest and longest continuously conducted health survey system in the world.
The crucial information gathered through this state-based telephone surveillance system is used by national, state, and local public health agencies to identify populations that might be most at risk and to monitor the need for and the effectiveness of various public health interventions.
Although the BRFSS is a useful tool for assessing coronary heart disease and stroke in adult populations, it has some limitations: it excludes people who do not have telephones or are in institutions such as nursing homes; it may under represent people who are severely impaired because of the functional capacity required to participate in the survey; and responses to BRFSS are self-reported and therefore have not been confirmed by a healthcare provider. Despite these limitations, the BRFSS is a uniquely powerful tool to provide the prevalence of coronary heart disease and stroke and related issues among older community-dwelling U.S. adults, due to its large sample size and proven reliability and validity.
The BRFSS is administered and supported by the Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. For more information, please visit https://www.cdc.gov/brfss.
Disclaimer: The mark “CDC” is owned by the U.S. Department of Health and Human Services (HHS) and is used with permission. Use of this logo is not an endorsement by HHS or the Centers for Disease Control and Prevention (CDC) or any particular product, service, or enterprise.





















.png)












No hay comentarios:
Publicar un comentario