
Scientists 'on the right track' toward universal flu vaccine
A research study into influenza virus transmission has offered new insights into the antibodies and immune responses that may protect against the influenza virus. The research could bring scientists a step closer to developing an effective, universal flu vaccine.
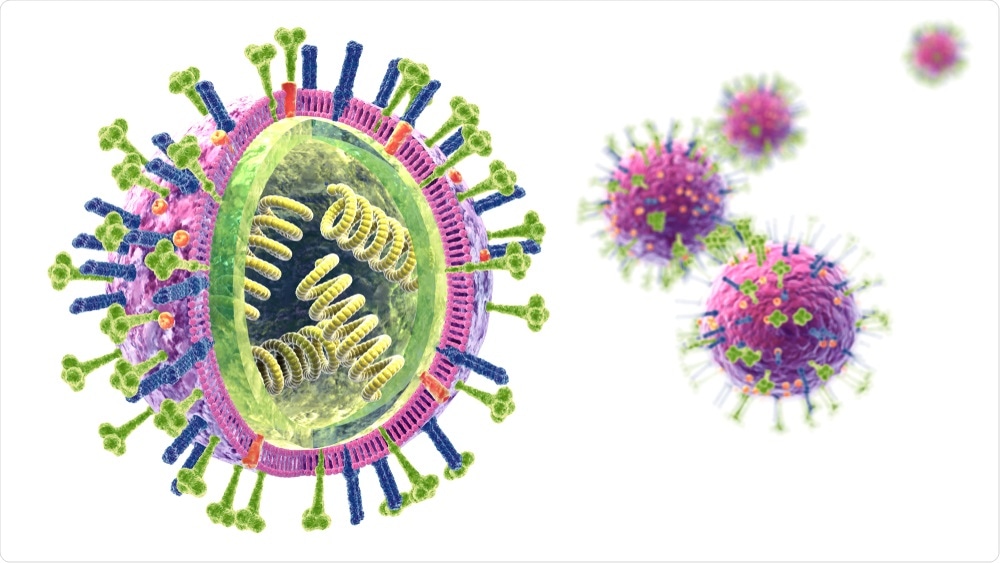 Axel_Koc | Shutterstock
Axel_Koc | ShutterstockThe influenza virus is responsible for up to 650,000 deaths each year, according to the study, which was published in Nature Medicine. The 2017-2018 flu season was very high in severity as reported by the Centers for Disease Control and Prevention (CDC), and showed elevated and geographically widespread influenza activity.
Two types of proteins called hemagglutinin (HA) and neuraminidase coat the flu virus (with this strain being called H1N1), and seasonal influenza vaccines currently target the head of the HA protein. This part of the protein changes regularly, and as such new vaccines are developed each season to target this specific area. The head of the protein is also targeted in laboratory tests to evaluate an individual’s immune response to different strains of the influenza virus.
However, this new study focused on the stem of the hemagglutinin protein, which does not change as often as the head of the protein and produces antibodies.
Aubree Gordon, a professor of epidemiology at U-M’s School of Public Health spoke on the importance of the study that was funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health.
Exploiting a viral weakness
The study explains that this approach has not been tested on humans, but showed success in animal studies, stating, “Antibodies against the hemagglutinin stalk confer protection in animal studies. However, no data exist on natural infections in humans.”
This is due to the controversial testing practice needed to gather human study data, which includes infecting healthy people with the influenza virus. Individuals used in influenza studies like this must also fit into specific requirements necessary for the test, narrowing the pool of potential participants. Accurately mimicking natural infection can also be difficult to achieve.
To circumvent these issues, the researchers conducting this new study carried out a “household transmission study […] in naturally exposed individuals.”
Researchers followed 88 people who had been infected with the H1N1 influenza A virus, and 300 of their household contacts in Nicaraguan families that had been followed by researchers for a number of years. When a member of the household contracted symptomatic influenza, blood samples were taken to test the rest of the household for the infection.
Researchers measured the pre-existing HA stem antibody levels in the household contacts with an enzyme-linked immunosorbent assay (ELISA) blood tests, with extra blood tests being taken after a period of 30 to 45 days.
Tracking the spread of the flu
To track whether household contacts became infected with influenza, nasal and throat swabs were also collected at the beginning of the study and then every two weeks.
Out of the 300 household contacts, 28 percent became infected with the influenza virus, and 63 percent of these household contacts developed symptomatic influenza.
The aim was to investigate who became infected, and who became sick from the virus. Professor Gordon explained the methods in more detail.
“Once someone in the house has been diagnosed, we go into the household very rapidly and then we followed them for two weeks to see who gets the flu. That way, we can get a blood sample and measure antibody levels pre-exposure and then see if they get infected (and if) they get sick.”
It was discovered that individuals with higher levels of HA stem antibodies were less likely to become infected by the virus. Generally, an antibody concentration of 1:40 indicates that 50 percent of people that have that level of antibody concentration will be protected from the influenza virus.
The study found that a fourfold increase in the amount of stem antibody levels showed a 42 percent reduction in influenza infection rates.
Researchers concluded that the level of HA stem antibodies may be used as a method of protection from influenza.
Florian Krammer, a professor of microbiology at the Icahn School of Medicine at Mount Sinai where the data analysis for the study was carried out, was positive about the direction the study’s results were taking influenza vaccine research.
“While there are caveats and further studies needed, this is good news for the development of stalk-based universal influenza virus vaccines. It seems we are on the right track,” he said.
“An additional finding of this study is that ELISA based readouts can be used as independent correlate of protection. ELISAs are binding assays and do not indicate functionality, but are much easier and quicker than functional assays.”
The study summarizes: “We found that hemagglutinin stalk antibodies are an independent correlate of protection from pandemic H1N1 infection and disease in a natural transmission setting. Further, antibodies measured by ELISA can be used as a powerful correlate of protection and to assess seroconversion, which will be important for novel universal influenza virus vaccine development.”
The researchers note that further studies will be needed to investigate the role of these antibodies in protecting against influenza A (H3N2) and influenza B.
Source:
NG, S., et al. (2019). Novel correlates of protection against pandemic H1N1 influenza A virus infection. Nature Medicine. doi.org/10.1038/s41591-019-0463-x.






















.png)












No hay comentarios:
Publicar un comentario