
Wisdom Teeth Removal
Wisdom teeth are the last teeth to erupt in permanent human dentition. Wisdom teeth removal is a surgical process to remove unwanted third molar teeth which are causing pain or damage to the gums.
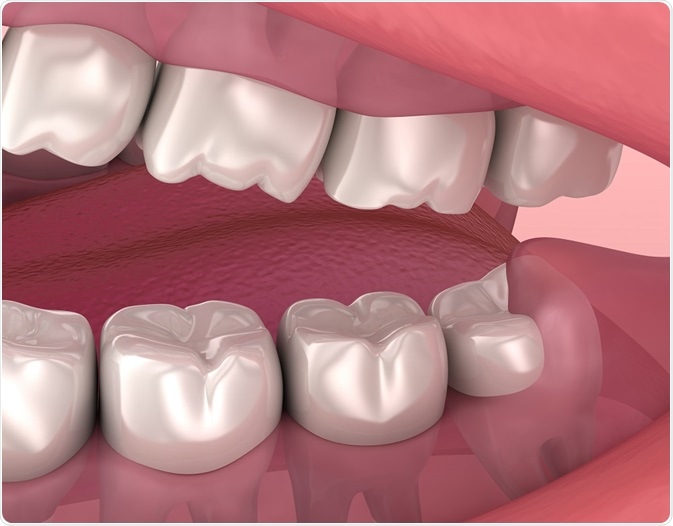
Alex Mit | Shutterstock
Inappropriately positioned wisdom teeth pose damage to the adjacent teeth or surrounding structures, hence, they require surgical removal.
Indications for the removal of wisdom teeth
There are many potential reasons why wisdom teeth need to be removed. Below is the list of various situations when the extraction of these teeth is recommended:
Frequent pain, infection or pericoronitis
Pericoronitis is referred to as inflammation of the gums/gingiva surrounding the partially erupted teeth. Pericoronitis can manifest in both acute and chronic forms. Partially erupted third molars usually lead to chronic recurring episodes of pericoronitis.
Patients usually experience excruciating pain and analgesics and antibiotic therapy alone fail to relieve symptoms of pericoronitis. Removal of wisdom teeth is a permanent cure for recurring pericoronitis.
A deep pocket leading to gum damage
A partially erupted the third molar makes a room for the food particles to reside in between the gum and the tooth, which leads to the formation of a periodontal pocket.
Periodontal pockets usually develop on the distal side of second molar teeth and a recurrent pocket formation can lead to pain, bleeding and at times also result in potential problems like bone loss. Hence, it is advisable to remove partially erupted third molars.
To create space in the dental arch for aligning the misaligned teeth
Impacted wisdom teeth acquire space in a narrow dental arch. Misaligned teeth are usually corrected with the help of braces. An orthodontist (a dentist who specializes in aligning the misaligned teeth) may recommend the removal of third molar teeth prior to an orthodontic treatment. Removal of impacted teeth creates more room for proper alignment of misaligned teeth.
Prevention of tooth cavities and root resorption
Third molar teeth lie at the back of the mouth. During brushing it becomes difficult to access and clean them. This makes third molars more predisposed to cavities and can also lead to the root resorption and cavity formation in the adjacent tooth. To prevent such complications it is advisable to remove partially erupted third molars.
Management of associated pathologies
Impacted third molars may give rise to odontogenic cysts and tumors; however it occurs rarely. These cysts and tumors are usually asymptomatic and are usually discovered accidently during an X-ray or during histopathological examination. To prevent any further complication it is advisable to remove third molar.
Before fabrication of a prosthesis
Impacted third molars may hinder the proper fitting of the prosthesis such as dentures. A prosthodontist may recommend the removal of impacted third molars before fabricating prosthesis in such patients.
For a removable prosthesis, at least 1 to 2 mm of bone is required between the tooth and the prosthesis to prevent irritation and resultant infection. Hence, it is advisable to remove third molars before fabricating a denture.
Prior to orthognathic surgeries
Orthognathic surgeries are done to correct the skeletal deformities. These surgeries are performed to correct mastication, speech, aesthetics and overall symmetry of the jaw bones. Dentists usually remove impacted third molars prior to such surgeries to avoid any interference during the surgical procedures.
Steps and procedure in wisdom teeth removal
Preparation prior to surgery
Complex wisdom tooth extractions are performed by an oral and maxillofacial surgeon. Patient’s medical history is studied before the surgery and a careful evaluation of the target tooth is done with specialized radiographs like intraoral periapical (IOPA) and orthopantomogram (OPG).
Diagnostic tests like a complete blood count, clotting and bleeding time are checked to prevent any complication and blood loss during surgery. Prior to the surgery, vitals of the patient are observed, and a local anesthetic is administered in minute amounts to check for allergic reactions.
1. Isolate the operative site
It is a three-step procedure and involves scrubbing and painting the skin oral mucosa (lining) with a cetrimide and povidone and iodine solution. However, scrubbing is done only on the skin, rinsing the skin with a normal saline solution to remove any soap residues, and painting the skin with a povidone-iodine solution to prevent the growth of microbes.
2. Administer anesthesia
Post the isolation process, the dentist injects anesthesia. There are two types of anesthesia namely local anesthesia and general anesthesia. Local anesthesia is the most common form of anesthesia injected to remove impacted teeth. This form of anesthesia is injected into the nerve supplying the tooth or around the area surrounding the tooth. The patient remains conscious during the surgical procedure.
Under some medical situations general anesthesia is given either via an intravenous route or by inhalation. The patient is unconscious at the time of surgery.
3. Incision of the gum tissue
The gum tissue is incised and the flap is raised to expose the bone and the tooth. This allows visibility of the impacted tooth to be removed. Dentists employ different types of flap designs for a speedy post operative healing, to minimize pain, swelling and infection. For removing mandibular (lower jaw) third molars mucoperiosteal flap is raised. Some other types of flaps are a buccal envelope flap and a triangular three-cornered flap.
4. Post-incision
Overlying bone above the impacted third molar is done either with chisel and mallet (hand instruments) or with dental burs. Usually a round bur is employed for gross bone removal. The alveolar bone overlying the tooth is shaved in way to create an appropriate groove; however it is ensured that minimal bone loss should occur during the process as it promotes faster post operative healing. Bone removal allows the access to the target tooth.
5. Sectioning of the tooth
Once the tooth is accessed it is divided into sections. Sectioning the tooth is important as it safely removes the tooth with minimal trauma. The number of sections in a tooth usually depends on various factors such as number and shape of the roots. At times the anatomy of nearby nerve is also considered while sectioning the tooth. Tooth sectioning easily removes the tooth from the socket.
6. The surgical site is cleaned
Surgical site is more susceptible to various infections, which may further complicate the healing process. Post closing the surgical site with stitches surgical site is properly cleansed to minimize the chances of infection. The patient is also advised not to touch the site to prevent any infection. Finally, gauze is placed over the stitches to manage any bleeding.
Sources:
- https://www.nhs.uk/conditions/wisdom-tooth-removal/what-happens/
- www.mayoclinic.org/.../pac-20395268
- https://www.healthlinkbc.ca/health-topics/tm6328
- www.mayoclinic.org/.../faq-20058558
- www.animated-teeth.com/wisdom_teeth/t2_wisdom_tooth_extraction.htm
- pdfs.semanticscholar.org/5997/d2d0ca5e0906f2f71bf09c307b487383339f.pdf
- http://podj.com.pk/archive/Jun_2014/PODJ-14.pdf
- https://www.toothiq.com/dental-procedure/surgical-tooth-extractions/
- https://www.iasj.net/iasj?func=fulltext&aId=70064
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4979926/
- https://jada.ada.org/article/S0002-8177(14)60117-3/pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907590/
Further Reading
Last Updated: Dec 3, 2018



































No hay comentarios:
Publicar un comentario