 |
| MMWR Weekly Vol. 65, No. 41 October 21, 2016 |
| PDF of this issue |
National Progress Toward Hepatitis C Elimination — Georgia, 2015–2016
Weekly / October 21, 2016 / 65(41);1132–1135
Lia Gvinjilia, MD, PhD1; Muazzam Nasrullah, MD, PhD2; David Sergeenko, MD3; Tengiz Tsertsvadze, MD, PhD4; George Kamkamidze, MD, PhD5; Maia Butsashvili, MD, PhD5; Amiran Gamkrelidze, MD, PhD6; Paata Imnadze, MD, PhD6; Valeri Kvaratskhelia3; Nikoloz Chkhartishvili, MD, PhD4; Lali Sharvadze, MD, PhD7; Jan Drobeniuc, MD, PhD2; Liesl Hagan, MPH2; John W. Ward, MD2; Juliette Morgan, MD8; Francisco Averhoff, MD2 (View author affiliations)
View suggested citationSummary
What is already known about this topic?Georgia is among the countries worldwide with the highest prevalence of hepatitis C virus (HCV) infection. The recent availability of highly effective, direct-acting antivirals (DAAs) capable of curing >90% of persons treated has made HCV elimination a possibility. On April 28, 2015, Georgia committed to an elimination plan, embarking on an ambitious program that included HCV screening and provision of curative treatment at no cost to infected persons.
What is added by this report?During the first year of the HCV elimination program in Georgia, 27,392 persons enrolled in the treatment program, and 8,448 initiated treatment with DAAs. Most persons (92.8%) who began treatment had advanced liver disease. Among 2,398 persons who completed treatment and were tested to determine treatment response, >80% were cured of their HCV infection. Georgia is developing a comprehensive HCV elimination plan that will include prevention and enhanced screening and linkage to care, with the goal of reaching HCV elimination by 2020.
What are the implications for public health practice?Substantial progress has been made to eliminate HCV infection in Georgia, and the country has demonstrated the ability for rapidly scale up of care and treatment services. To achieve elimination, substantial challenges remain, including increasing access to care and treatment services and implementing a comprehensive approach to prevention and control of HCV infection. Georgia’s HCV elimination program could provide lessons for future programs to control HCV infection worldwide, particularly as treatment becomes more affordable and more countries seek to provide care and treatment services.
Lia Gvinjilia, MD, PhD1; Muazzam Nasrullah, MD, PhD2; David Sergeenko, MD3; Tengiz Tsertsvadze, MD, PhD4; George Kamkamidze, MD, PhD5; Maia Butsashvili, MD, PhD5; Amiran Gamkrelidze, MD, PhD6; Paata Imnadze, MD, PhD6; Valeri Kvaratskhelia3; Nikoloz Chkhartishvili, MD, PhD4; Lali Sharvadze, MD, PhD7; Jan Drobeniuc, MD, PhD2; Liesl Hagan, MPH2; John W. Ward, MD2; Juliette Morgan, MD8; Francisco Averhoff, MD2 (View author affiliations)
View suggested citation
The country of Georgia has a high prevalence of hepatitis C virus (HCV) infection, associated with exposures to HCV in health care settings with inadequate infection control and unsafe injections among persons who inject drugs (1). In April 2015, in collaboration with CDC and other partners, Georgia embarked on a program to eliminate HCV infection, subsequently defined as achieving a 90% reduction in prevalence by 2020. The initial phase of the program focused on providing HCV treatment to infected persons with advanced liver disease and at highest risk for HCV-associated morbidity and mortality. By April 27, 2016, a total of 27,392 HCV-infected persons registered for the program, 8,448 (30.8%) started treatment, and 5,850 patients (69.2%) completed HCV treatment. Among patients completing treatment who were eligible for posttreatment testing, 2,398 received polymerase chain reaction (PCR) testing for HCV at least 12 weeks after completion of treatment; 1,980 (82.6%) had no detectable virus, indicative of a sustained virologic response* (i.e., cure). Major challenges to achieving elimination remain, including the need to increase access to care and treatment services and implement a comprehensive approach to prevention and control of HCV infection. As a global leader in this effort, the Georgia HCV Elimination Program can help pave the way for other countries experiencing high rates of HCV infection to undertake similar initiatives.
Georgia is a country with a population of 3.7 million (2) and borders the Black Sea, Russia, Turkey, Armenia, and Azerbaijan. Results from a serosurvey conducted in 2015 among adults found an estimated HCV infection prevalence (i.e., tested HCV-antibody positive) of 7.7% (5.4% tested positive for active infection by PCR) (Georgia Ministry of Labor, Health, and Social Affairs [MoLHSA], unpublished data, 2016). With strong stakeholder support, including partnership and technical assistance from CDC, and commitment from Gilead Sciences to donate direct-acting antiviral HCV medications (DAAs), Georgia embarked on the world’s first HCV elimination program on April 28, 2015 (1). Initially, four treatment centers located in Tbilisi (Georgia’s capital) provided HCV treatment to program participants. By April 27, 2016, the number of treatment centers had increased to 17 and they were located throughout the country, with staff members that included 95 physicians and infectious disease specialists or gastroenterologists providing HCV treatment services. All patients had access to point-of-care and laboratory-based HCV antibody testing, viral load determination, and genotyping. Noninvasive tests used to determine the degree of hepatic fibrosis included the following: FIB-4 score, which combines age and standard blood tests (platelet count, alanine aminotransferase, aspartate aminotransferase) (3), and ultrasound or transient elastography, which measures the decrease in tissue elasticity that accompanies liver fibrosis (4,5). Genotyping was performed for all patients who tested positive for HCV by PCR. Six major genotypes of HCV are recognized worldwide, and treatment of HCV infection varies by genotype (6). Patients with advanced liver disease (F3 or F4 by METAVIR† fibrosis score) were prioritized to receive treatment during the first year of the program.
A sliding-scale approach was used for diagnostics and clinical monitoring, with patients charged based on their ability to pay and the local government or MoLHSA paying the balance. All program participants received sofosbuvir-based treatment regimens, provided free-of-charge by Gilead Sciences; the Georgian government purchased additional medications (i.e., pegylated interferon and ribavirin) and provided them at no cost to patients for whom such treatment was indicated.
During April 28, 2015–April 27, 2016, a total of 27,392 patients with evidence of HCV infection (positive HCV antibody test results) had enrolled in the program. The number of enrollees peaked during the first month of the program and generally declined over time (Figure 1). The number of patients initiating HCV treatment in the country increased linearly during the year, to a total of 8,448 (Figure 2). Of those enrolled, 27,155 (99.1%) initiated diagnostic workup, including confirmation of active HCV infection and assessment of hepatic fibrosis to determine eligibility for treatment. Among those enrolled in the program, 9,615 (36.3%) completed diagnostic workup, and 8,448 (87.9%) initiated treatment for HCV (Figure 3). Most patients treated (92.8%) met advanced liver disease criteria. The most common treatment regimens were sofosbuvir in combination with ribavirin (45.4%), and sofosbuvir in combination with ribavirin and pegylated interferon (33.9%).
Outcome data for patients treated through April 2016 indicated that among 2,398 persons eligible for a sustained virologic response determination 12 weeks after completion of treatment and who were tested for the presence of HCV RNA, levels of HCV RNA were undetectable in 1,980 (82.6%) of those tested, indicating a virologic cure. Among those completing their course of treatment who were tested, cure rates were lowest among genotype 1 patients (72.6%; 724 of 997 patients), intermediate among those infected with genotype 2 (84.7%; 421 of 497), and highest among those with genotype 3 (92.4%; 834 of 903). Among the 8,448 who initiated treatment, 325 (3.8%), did not complete the treatment course; 173 of the 325 patients died, and 80 discontinued treatment because of an adverse event.
In mid-February 2016, Gilead Sciences began providing (free-of-charge) the newer ledipasvir/sofosbuvir DAA combination drug regimen to the program. Among participants who initiated treatment in the first year, 11.7% (n = 985) received the new regimen. This included 162 persons who restarted treatment with ledipasvir/sofosbuvir after introduction of this combination DAA for various reasons, primarily failure to achieve viral clearance after initial treatment course (n = 155). Treatment outcome data are not available for patients receiving this combination therapy.
Discussion
The Georgia HCV Elimination Program made substantial progress in its first year. Since the launch of the program in April 2015, 27,392 HCV-infected persons were enrolled and 8,448 initiated treatment, which represents a >400% increase in the number treated compared with the total number of HCV-infected persons treated in the country during the previous 4 years (1). Persons with advanced liver disease, who are at highest risk for morbidity and mortality, were prioritized for treatment during the first year, and >90% of those treated met this criteria as determined by ultrasound or transient elastography. Rates of virologic cure were >80% among this population. The effect on prevalence of active HCV infection, estimated at 5.4% in 2015, will be reassessed in several years as the HCV elimination program progresses and treatment coverage expands, curing most Georgians currently living with HCV infection. Georgia has taken a collaborative, informed approach to eliminating HCV infection. Together with CDC, the World Health Organization (WHO), and other international partners, Georgia’s MoLHSA developed a technical advisory group (TAG), which convened its first meeting in November 2015. To help Georgia reach its proposed elimination goals, TAG recommended that MoLHSA address gaps in advocacy and awareness; surveillance; prevention of transmission, including harm reduction; blood safety; infection control in health and non–health care settings; and evidence-based screening and linkage to care (7). Several strategies were proposed at the meeting, including assessing Georgia’s prevalence of disease and risk factors for transmission; implementing measures to prevent transmission; identifying all persons living with HCV infection; and providing patients with access to high-quality diagnostics and free treatment with DAA medications. In response to TAG recommendations and collaboration with CDC, Georgia’s MoLHSA is developing a comprehensive HCV elimination plan to address important challenges and outline steps and strategies for enhanced screening and linkage-to-care activities, expansion of HCV treatment to reach populations at high risk for infection, and development of a surveillance system to assess progress toward achieving elimination goals.
Despite notable progress during the last year, major challenges remain. To ensure high-quality screening and monitoring as the program expands, a laboratory quality assurance and quality control system covering all treatment centers is needed. To monitor progress toward elimination goals, surveillance systems capable of capturing data from affected populations and those with acute disease are needed, allowing for monitoring trends and risk factors for infection. Collection of quality and timely treatment data is important to monitor the progress of the care and treatment program. These gaps will be addressed in Georgia’s comprehensive HCV elimination plan, which is currently under development. As the HCV treatment program continues to expand and the number of providers and sites that provide HCV care and treatment services grows, the capacity of the information system will need to be increased. Georgia’s MoLHSA is anticipating this growth and is working with partners to ensure the system is upgraded to handle additional demands.
In its first year, Georgia’s HCV elimination program primarily served patients who already knew their infection status, voluntarily came to participating clinics, and enrolled in the program. However, most persons living with HCV infection are unaware of their HCV infection and consequently are not participating in the program and not receiving care and treatment. Georgia is developing a comprehensive plan that will increase patient testing, ensure that tested patients are informed of their test results, and ensure that those who test positive for HCV antibodies are provided confirmatory testing and if infected, linked to care and treatment services. As more Georgians are tested for HCV, the demand for treatment will increase. Primary care providers and settings serving populations at high risk (e.g., centers providing services such as opioid substitution therapy and needle and syringe provision to people who inject drugs) need to be prepared to provide HCV treatment, as the demand for therapy is anticipated to exceed the current capacity of providers offering treatment (i.e., infectious disease specialists and gastroenterologists).
In the near future, Georgians will likely have access to even newer DAAs associated with high rates of virologic cure regardless of HCV genotype, suggesting that genotype testing might not remain a prerequisite for treatment. Use of these antiviral medications is expected to simplify HCV diagnostics and patient management and monitoring in Georgia, allowing more patients to receive timely treatment. In many low-to-middle income countries with a high prevalence of HCV infection, access to advanced diagnostics is limited. Specific models of care and treatment that use simplified testing and patient management are needed to demonstrate feasibility of HCV-related care and treatment in resource-limited settings like Georgia.
The World Health Assembly endorsed the WHO strategic framework for hepatitis prevention that includes goals for the elimination of hepatitis C as a public health threat by 2030, with interim measures by 2020 (8). Georgia’s HCV elimination program model could provide important lessons for future initiatives to control HCV infection worldwide, particularly as testing is simplified, treatment becomes more affordable, and more countries seek to address the growing prevalence of HCV infection.
Corresponding author: Muazzam Nasrullah, snasrullah@cdc.gov, 404-639-3271.
1CDC Foundation, Tbilisi, Georgia; 2Division of Viral Hepatitis, National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, CDC; 3Ministry of Labor Health and Social Affairs of Georgia, Tbilisi, Georgia; 4Infectious Diseases, AIDS, and Clinical Immunology Research Center, Tbilisi, Georgia; 5Neolab, Tbilisi, Georgia; 6National Center for Disease Control and Public Health of Georgia, Tbilisi, Georgia; 7Joint Georgian-French Hepatology Clinic Hepa, Tbilisi, Georgia; 8Global Disease Detection, Division of Global Health Protection, South Caucasus CDC Office, Tbilisi, Georgia.
* Sustained virologic response is defined as undetectable (or below the lower limit of quantification) HCV RNA at 12–24 weeks after cessation of treatment (Wedemeyer H, et al., http://onlinelibrary.wiley.com/doi/10.1002/hep.25888/pdf).
† The METAVIR score is a semiquantitative classification system that consists of an activity score and a fibrosis score, specifically designed and validated for patients with HCV (Bedossa P, et al., http://onlinelibrary.wiley.com/doi/10.1002/hep.510240201/pdf).
References
- Mitruka K, Tsertsvadze T, Butsashvili M, et al. Launch of a nationwide hepatitis C elimination program—Georgia, April 2015. MMWR Morb Mortal Wkly Rep 2015;64:753–7. CrossRefPubMed
- National Statistics Office of Georgia. Main statistics: population. Tbilisi, Georgia: National Statistics Office of Georgia; 2016. http://geostat.ge/index.php?action=page&p_id=152&lang=eng
- Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and fibrotest. Hepatology 2007;46:32–6.CrossRef PubMed
- Talwalkar JA, Kurtz DM, Schoenleber SJ, West CP, Montori VM. Ultrasound-based transient elastography for the detection of hepatic fibrosis: systematic review and meta-analysis. Clin Gastroenterol Hepatol 2007;5:1214–20. CrossRef PubMed
- Afdhal NH. Fibroscan (transient elastography) for the measurement of liver fibrosis. Gastroenterol Hepatol (N Y) 2012;8:605–7. PubMed
- Smith DB, Bukh J, Kuiken C, et al. Expanded classification of hepatitis C virus into 7 genotypes and 67 subtypes: updated criteria and genotype assignment web resource. Hepatology 2014;59:318–27. CrossRef PubMed
- Ministry of Labour Health and Social Affairs of Georgia. Hepatitis Technical Advisory Group (TAG) recommendations for achieving the 2020 goals towards eliminating hepatitis C infection in the country of Georgia. Tbilisi, Georgia: Ministry of Labour Health and Social Affairs of Georgia; 2015. http://www.moh.gov.ge/files//2016/Failebi/09.06.16-1.pdf
- World Health Organization. Draft global health sector strategies: viral hepatitis, 2016–2021. Geneva, Switzerland: World Health Organization; 2016. http://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_32-en.pdf?ua=1
 FIGURE 1. Number of persons with positive hepatitis C virus (HCV) results enrolling in treatment program, by month — nationwide HCV elimination program, Georgia, April 2015–April 2016*
FIGURE 1. Number of persons with positive hepatitis C virus (HCV) results enrolling in treatment program, by month — nationwide HCV elimination program, Georgia, April 2015–April 2016*
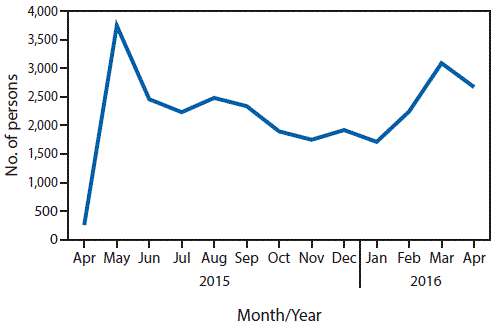
Source: Georgia Ministry of Labor, Health, and Social Affairs.
* The number of clinical sites increased from four in April 2015 to 17 in April 2016.
 FIGURE 2. Cumulative number of persons (N = 8,448) with positive hepatitis C virus (HCV) results who started HCV treatment, by month — nationwide HCV elimination program, Georgia, May 14, 2015–April 27, 2016
FIGURE 2. Cumulative number of persons (N = 8,448) with positive hepatitis C virus (HCV) results who started HCV treatment, by month — nationwide HCV elimination program, Georgia, May 14, 2015–April 27, 2016
Source: Georgia’s HCV Elimination Program Treatment Database.
 FIGURE 3. Cascade of care for hepatitis C virus (HCV)-infected patients — nationwide HCV elimination program, Georgia, April 28, 2015–April 27, 2016*,†
FIGURE 3. Cascade of care for hepatitis C virus (HCV)-infected patients — nationwide HCV elimination program, Georgia, April 28, 2015–April 27, 2016*,†
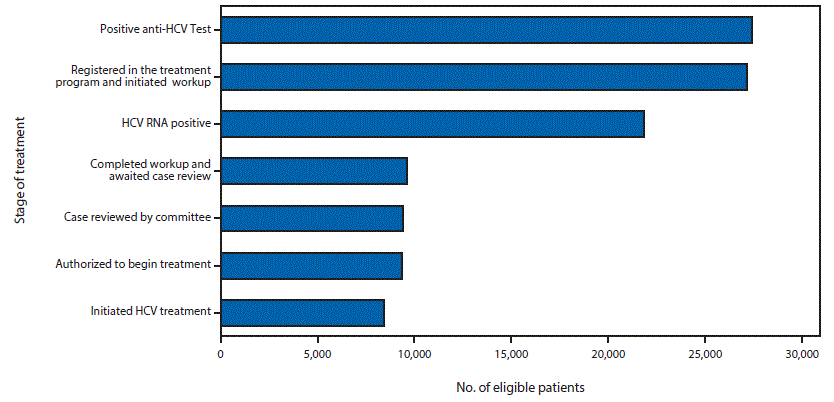
Abbreviation: MOLHSA = Ministry of Labor, Health, and Social Affairs; STOP-C = HCV Elimination Program Treatment Database.
*Patients with positive anti-HCV test began treatment at one of 17 provider sites; data from MOLHSA’s financial reimbursement system.
† Of the patients who initiated HCV treatment, 162 (1.9%) with different indications have restarted HCV treatment.





















.png)












No hay comentarios:
Publicar un comentario