
Interim Additional Guidance for Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed COVID-19 in Outpatient Hemodialysis Facilities — This guidance is provided to clarify SARS-CoV-2 infection prevention and control (IPC) recommendations that are specific to outpatient hemodialysis facilities. This information complements, but does not replace, the general CDC IPC recommendations for SARS-CoV-2 available in Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.
Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic
Summary of Changes to the Guidance
Below are changes to the guidance as of July 15, 2020:
- Added language that protective eyewear (e.g., safety glasses, trauma glasses) with gaps between glasses and the face likely do not protect eyes from all splashes and sprays.
Background
This interim guidance has been updated based on currently available information about COVID-19 and the current situation in the United States. As healthcare facilities begin to relax restrictions on healthcare services provided to patients (e.g., restarting elective procedures), in accordance with guidance from local and state officials, there are precautions that should remain in place as a part of the ongoing response to the COVID-19 pandemic. Most recommendations in this updated guidance are not new (except as noted in the summary of changes above); they have been reorganized into the following sections:
- Recommended infection prevention and control (IPC) practices for routine healthcare delivery during the pandemic
- Recommended IPC practices when caring for a patient with suspected or confirmed SARS-CoV-2 infection
This guidance is applicable to all U.S. healthcare settings. This guidance is not intended for non-healthcare settings (e.g., schools) OR for persons outside of healthcare settings. For information regarding modes of transmission, clinical management, air or ground medical transport, or laboratory settings, refer to the COVID-19 website.
Additional Key Resources:
- Strategies to Optimize the Supply of PPE and Equipment
- Criteria for Return to Work for Healthcare Personnel with Suspected or Confirmed COVID-19 (Interim Guidance)
- Strategies to Mitigate Healthcare Personnel Staffing Shortages
- Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to Coronavirus Disease 2019 (COVID-19)
- Discontinuation of Transmission-Based Precautions and Disposition of Patients with COVID-19 in Healthcare Settings (Interim Guidance)
1. Recommended routine infection prevention and control (IPC) practices during the COVID-19 pandemic
CDC recommends using additional infection prevention and control practices during the COVID-19 pandemic, along with standard practices recommended as a part of routine healthcare delivery to all patients. These practices are intended to apply to all patients, not just those with suspected or confirmed SARS-CoV-2 infection (See Section 2 for additional practices that should be used when caring for patients with suspected or confirmed SARS-CoV-2 infection).
These additional practices include:
Implement Telehealth and Nurse-Directed Triage Protocols
- Continue to use telehealth strategies to provide high-quality patient care and reduce the risk of SARS-CoV-2 transmission in healthcare settings.
- When scheduling appointments for routine medical care (e.g., annual physical, elective surgery), instruct patients to call ahead and discuss the need to reschedule their appointment if they have symptoms of COVID-19 on the day they are scheduled to be seen.
- If they don’t have symptoms of COVID-19, advise them that they should still put on their own cloth face covering before entering the facility.
- When scheduling appointments for patients requesting evaluation for possible SARS-CoV-2 infection, use nurse-directed triage protocols to determine if an appointment is necessary or if the patient can be managed from home.
- If the patient must come in for an appointment, instruct them to call beforehand to inform triage personnel that they have symptoms of COVID-19 and to take appropriate preventive actions (e.g., follow triage procedures, put on their own cloth face covering prior to entry and throughout their visit or, if a cloth face covering cannot be tolerated, hold a tissue against their mouth and nose to contain respiratory secretions).
Screen and Triage Everyone Entering a Healthcare Facility for Signs and Symptoms of COVID-19
Although screening for symptoms will not identify asymptomatic or pre-symptomatic individuals with SARS-CoV-2 infection, symptom screening remains an important strategy to identify those who could have COVID-19 so appropriate precautions can be implemented.
- Take steps to ensure that everyone adheres to source control measures and hand hygiene practices while in a healthcare facility
- Post visual alerts (e.g., signs, posters) at the entrance and in strategic places (e.g., waiting areas, elevators, cafeterias) to provide instructions (in appropriate languages) about wearing a cloth face covering or facemask for source control and how and when to perform hand hygiene.
- Provide supplies for respiratory hygiene and cough etiquette, including alcohol-based hand sanitizer (ABHS) with 60-95% alcohol, tissues, and no-touch receptacles for disposal, at healthcare facility entrances, waiting rooms, and patient check-ins.
- Limit and monitor points of entry to the facility.
- Consider establishing screening stations outside the facility to screen individuals before they enter.
- Screen everyone (patients, HCP, visitors) entering the healthcare facility for symptoms consistent with COVID-19 or exposure to others with SARS-CoV-2 infection and ensure they are practicing source control.
- Actively take their temperature and document absence of symptoms consistent with COVID-19. Fever is either measured temperature ≥100.0°F or subjective fever.
- Ask them if they have been advised to self-quarantine because of exposure to someone with SARS-CoV-2 infection.
- Properly manage anyone with symptoms of COVID-19 or who has been advised to self-quarantine:
- HCP should return home and should notify occupational health services to arrange for further evaluation.
- Visitors should be restricted from entering the facility.
- Patients should be isolated in an examination room with the door closed.
- If an examination room is not immediately available, such patients should not wait among other patients seeking care.
- Identify a separate, well-ventilated space that allows waiting patients to be separated by 6 or more feet, with easy access to respiratory hygiene supplies.
- In some settings, patients might opt to wait in a personal vehicle or outside the healthcare facility where they can be contacted by mobile phone when it is their turn to be evaluated.
- Depending on the level of transmission in the community, facilities might also consider designating a separate area at the facility (e.g., an ancillary building or temporary structure) or nearby location as an evaluation area where patients with symptoms of COVID-19 can seek evaluation and care.
Re-evaluate admitted patients for signs and symptoms of COVID-19
While screening should be performed upon entry to the facility, it should also be incorporated into daily assessments of all admitted patients. All fevers and symptoms consistent with COVID-19 among admitted patients should be properly managed and evaluated (e.g., place any patient with unexplained fever or symptoms of COVID-19 on appropriate Transmission-Based Precautions and evaluate).
Implement Universal Source Control Measures
Source control refers to use of cloth face coverings or facemasks to cover a person’s mouth and nose to prevent spread of respiratory secretions when they are talking, sneezing, or coughing. Because of the potential for asymptomatic and pre-symptomatic transmission, source control measures are recommended for everyone in a healthcare facility, even if they do not have symptoms of COVID-19.
- Patients and visitors should, ideally, wear their own cloth face covering (if tolerated) upon arrival to and throughout their stay in the facility. If they do not have a face covering, they should be offered a facemask or cloth face covering, as supplies allow.
- Patients may remove their cloth face covering when in their rooms but should put it back on when around others (e.g., when visitors enter their room) or leaving their room.
- Facemasks and cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or anyone who is unconscious, incapacitated or otherwise unable to remove the mask without assistance.
- HCP should wear a facemask at all times while they are in the healthcare facility, including in breakrooms or other spaces where they might encounter co-workers.
- When available, facemasks are preferred over cloth face coverings for HCP as facemasks offer both source control and protection for the wearer against exposure to splashes and sprays of infectious material from others.
- Cloth face coverings should NOT be worn instead of a respirator or facemask if more than source control is needed.
- To reduce the number of times HCP must touch their face and potential risk for self-contamination, HCP should consider continuing to wear the same respirator or facemask (extended use) throughout their entire work shift, instead of intermittently switching back to their cloth face covering.
- Respirators with an exhalation valve are not recommended for source control, as they allow unfiltered exhaled breath to escape.
- HCP should remove their respirator or facemask, perform hand hygiene, and put on their cloth face covering when leaving the facility at the end of their shift.
- When available, facemasks are preferred over cloth face coverings for HCP as facemasks offer both source control and protection for the wearer against exposure to splashes and sprays of infectious material from others.
- Educate patients, visitors, and HCP about the importance of performing hand hygiene immediately before and after any contact with their facemask or cloth face covering.
Encourage Physical Distancing
Healthcare delivery requires close physical contact between patients and HCP. However, when possible, physical distancing (maintaining 6 feet between people) is an important strategy to prevent SARS-CoV-2 transmission.
Examples of how physical distancing can be implemented for patients include:
- Limiting visitors to the facility to those essential for the patient’s physical or emotional well-being and care (e.g., care partner, parent).
- Encourage use of alternative mechanisms for patient and visitor interactions such as video-call applications on cell phones or tablets.
- Scheduling appointments to limit the number of patients in waiting rooms.
- Arranging seating in waiting rooms so patients can sit at least 6 feet apart.
- Modifying in-person group healthcare activities (e.g., group therapy, recreational activities) by implementing virtual methods (e.g., video format for group therapy) or scheduling smaller in-person group sessions while having patients sit at least 6 feet apart.
- In some circumstances, such as higher levels of community transmission or numbers of patients with COVID-19 being cared for at the facility, and when healthcare-associated transmission is occurring, facilities might cancel in-person group activities in favor of an exclusively virtual format.
For HCP, the potential for exposure to SARS-CoV-2 is not limited to direct patient care interactions. Transmission can also occur through unprotected exposures to asymptomatic or pre-symptomatic co-workers in breakrooms or co-workers or visitors in other common areas. Examples of how physical distancing can be implemented for HCP include:
- Reminding HCP that the potential for exposure to SARS-CoV-2 is not limited to direct patient care interactions.
- Emphasizing the importance of source control and physical distancing in non-patient care areas.
- Providing family meeting areas where all individuals (e.g., visitors, HCP) can remain at least 6 feet apart from each other.
- Designating areas for HCP to take breaks, eat, and drink that allow them to remain at least 6 feet apart from each other, especially when they must be unmasked.
Implement Universal Use of Personal Protective Equipment
- HCP working in facilities located in areas with moderate to substantial community transmission are more likely to encounter asymptomatic or pre-symptomatic patients with SARS-CoV-2 infection. If SARS-CoV-2 infection is not suspected in a patient presenting for care (based on symptom and exposure history), HCP should follow Standard Precautions (and Transmission-Based Precautions if required based on the suspected diagnosis).
They should also:- Wear eye protection in addition to their facemask to ensure the eyes, nose, and mouth are all protected from exposure to respiratory secretions during patient care encounters.
- Wear an N95 or equivalent or higher-level respirator, instead of a facemask, for:
- Aerosol generating procedures (refer to Which procedures are considered aerosol generating procedures in healthcare settings FAQ) and
- Surgical procedures that might pose higher risk for transmission if the patient has COVID-19 (e.g., that generate potentially infectious aerosols or involving anatomic regions where viral loads might be higher, such as the nose and throat, oropharynx, respiratory tract) (refer to Surgical FAQ).
- Respirators with exhalation valves are not recommended for source control and should not be used during surgical procedures as unfiltered exhaled breath would compromise the sterile field.
- For HCP working in areas with minimal to no community transmission, HCP should continue to adhere to Standard and Transmission-Based Precautions, including use of eye protection and/or an N95 or equivalent or higher-level respirator based on anticipated exposures and suspected or confirmed diagnoses. Universal use of a facemask for source control is recommended for HCP.
Consider Performing Targeted SARS-CoV-2 Testing of Patients Without Signs or Symptoms of COVID-19
In addition to the use of universal PPE and source control in healthcare settings, targeted SARS-CoV-2 testing of patients without signs or symptoms of COVID-19 might be used to identify those with asymptomatic or pre-symptomatic SARS-CoV-2 infection and further reduce risk for exposures in some healthcare settings. Depending on guidance from local and state health departments, testing availability, and how rapidly results are available, facilities can consider implementing pre-admission or pre-procedure diagnostic testing with authorized nucleic acid or antigen detection assays for SARS-CoV-2.
Testing results might inform decisions about rescheduling elective procedures or about the need for additional Transmission-Based Precautions when caring for the patient. Limitations of using this testing strategy include obtaining negative results in patients during their incubation period who later become infectious and false negative test results, depending on the test method used.
Testing results might inform decisions about rescheduling elective procedures or about the need for additional Transmission-Based Precautions when caring for the patient. Limitations of using this testing strategy include obtaining negative results in patients during their incubation period who later become infectious and false negative test results, depending on the test method used.
Consider if elective procedures, surgeries, and non-urgent outpatient visits should be postponed in certain circumstances.
Facilities must balance the need to provide necessary services while minimizing risk to patients and HCP. Facilities should consider the potential for patient harm if care is deferred when making decisions about providing elective procedures, surgeries, and non-urgent outpatient visits. Refer to the Framework for Healthcare Systems Providing Non-COVID-19 Clinical Care During the COVID-19 Pandemic for additional guidance.
Optimize the Use of Engineering Controls and Indoor Air Quality
- Optimize the use of engineering controls to reduce or eliminate exposures by shielding HCP and other patients from infected individuals. Examples of engineering controls include:
- Physical barriers and dedicated pathways to guide symptomatic patients through triage areas.
- Remote triage facilities for patient intake areas.
- If climate permits, outdoor assessment and triage stations for patients with respiratory symptoms.
- Vacuum shrouds for surgical procedures likely to generate aerosols.
- Reassess the use of open bay recovery areas.
- Explore options to improve indoor air quality in all shared spaces.
- Optimize air-handling systems (ensuring appropriate directionality, filtration, exchange rate, proper installation, and up to date maintenance).
- Consider the addition of portable solutions (e.g., portable HEPA filtration units) to augment air quality in areas when permanent air-handling systems are not a feasible option.
Create a Process to Respond to SARS-CoV-2 Exposures Among HCP and Others
Healthcare facilities should have a process for notifying the health department about suspected or confirmed cases of SARS-CoV-2 infection, and should establish a plan, in consultation with local public health authorities, for how exposures in a healthcare facility will be investigated and managed and how contact tracing will be performed. The plan should address the following:
- Who is responsible for identifying contacts (e.g., HCP, patients, visitors) and notifying potentially exposed individuals?
- How will such notifications occur?
- What actions and follow-up are recommended for those who were exposed?
Contact tracing should be carried out in a way that protects the confidentiality of affected individuals and is consistent with applicable laws and regulations. HCP and patients who are currently admitted to the facility or were transferred to another healthcare facility should be prioritized for notification. These groups, if infected, have the potential to expose a large number of individuals at higher risk for severe disease, or in the situation of admitted patients, are at higher risk for severe illness themselves.
Information about when HCP with suspected or confirmed SARS-CoV-2 infection may return to work is available in the Interim Guidance on Criteria for Return to Work for Healthcare Personnel with Confirmed or Suspected COVID-19.
Information about risk assessment and work restrictions for HCP exposed to SARS-CoV-2 is available in the Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to Coronavirus Disease 2019 (COVID-19).
Healthcare facilities must be prepared for potential staffing shortages and have plans and processes in place to mitigate these, including providing resources to assist HCP with anxiety and stress. Strategies to mitigate staffing shortages are available.
2. Recommended infection prevention and control (IPC) practices when caring for a patient with suspected or confirmed SARS-CoV-2 infection
Establish Reporting within and between Healthcare Facilities and to Public Health Authorities
- Implement mechanisms and policies that promote situational awareness for facility staff including infection control, healthcare epidemiology, facility leadership, occupational health, clinical laboratory, and frontline staff about patients with suspected or confirmed SARS-CoV-2 infection and facility plans for response.
- Communicate and collaborate with public health authorities.
- Facilities should designate specific persons within the healthcare facility who are responsible for communication with public health officials and dissemination of information to HCP.
Patient Placement
- For patients with COVID-19 or other respiratory infections, evaluate need for hospitalization. If hospitalization is not medically necessary, home care is preferable if the individual’s situation allows.
- If admitted, place a patient with suspected or confirmed SARS-CoV-2 infection in a single-person room with the door closed. The patient should have a dedicated bathroom.
- Airborne Infection Isolation Rooms (AIIRs) (See definition of AIIR in appendix) should be reserved for patients who will be undergoing aerosol generating procedures (See Aerosol Generating Procedures Section).
- Personnel entering the room should use PPE as described below.
- As a measure to limit HCP exposure and conserve PPE, facilities could consider designating entire units within the facility, with dedicated HCP, to care for patients with suspected or confirmed SARS-CoV-2 infection. Dedicated means that HCP are assigned to care only for these patients during their shift.
- Determine how staffing needs will be met as the number of patients with suspected or confirmed SARS-CoV-2 infection increases and if HCP become ill and are excluded from work.
- It might not be possible to distinguish patients who have COVID-19 from patients with other respiratory viruses. As such, patients with different respiratory pathogens might be cohorted on the same unit. However, only patients with the same respiratory pathogen may be housed in the same room. For example, a patient with COVID-19 should ideally not be housed in the same room as a patient with an undiagnosed respiratory infection or a respiratory infection caused by a different pathogen.
- To the extent possible, patients with suspected or confirmed SARS-CoV-2 infection should be housed in the same room for the duration of their stay in the facility (e.g., minimize room transfers).
- Limit transport and movement of the patient outside of the room to medically essential purposes.
- Whenever possible, perform procedures/tests in the patient’s room.
- Consider providing portable x-ray equipment in patient cohort areas to reduce the need for patient transport.
- Communicate information about patients with suspected or confirmed SARS-CoV-2 infection to appropriate personnel before transferring them to other departments in the facility (e.g., radiology) and to other healthcare facilities.
- Patients should wear a facemask or cloth face covering to contain secretions during transport. If patients cannot tolerate a facemask or cloth face covering or one is not available, they should use tissues to cover their mouth and nose while out of their room.
- Once the patient has been discharged or transferred, HCP, including environmental services personnel, should refrain from entering the vacated room until sufficient time has elapsed for enough air changes to remove potentially infectious particles (more information on clearance rates under differing ventilation conditions is available). After this time has elapsed, the room should undergo appropriate cleaning and surface disinfection before it is returned to routine use.
Personal Protective Equipment
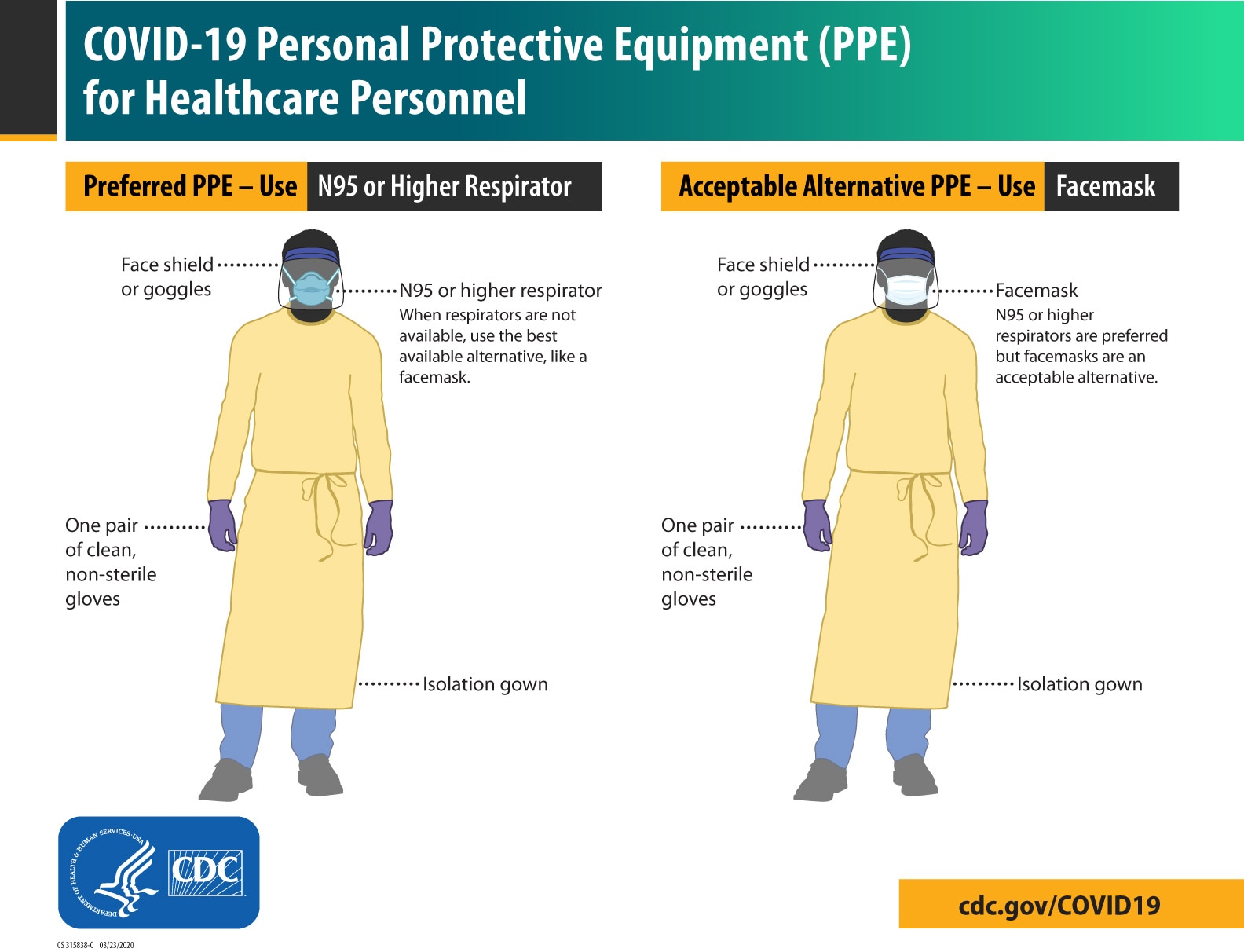
Download the Print-only PDF
HCP who enter the room of a patient with suspected or confirmed SARS-CoV-2 infection should adhere to Standard Precautions and use a NIOSH-approved N95 or equivalent or higher-level respirator (or facemask if a respirator is not available), gown, gloves, and eye protection.
When available, respirators (instead of facemasks) are preferred; they should be prioritized for situations where respiratory protection is most important and the care of patients with pathogens requiring Airborne Precautions (e.g., tuberculosis, measles, varicella). Information about the recommended duration of Transmission-Based Precautions is available in the Interim Guidance for Discontinuation of Transmission-Based Precautions and Disposition of Hospitalized Patients with COVID-19.
- Hand Hygiene
- HCP should perform hand hygiene before and after all patient contact, contact with potentially infectious material, and before putting on and after removing PPE, including gloves. Hand hygiene after removing PPE is particularly important to remove any pathogens that might have been transferred to bare hands during the removal process.
- HCP should perform hand hygiene by using ABHS with 60-95% alcohol or washing hands with soap and water for at least 20 seconds. If hands are visibly soiled, use soap and water before returning to ABHS.
- Healthcare facilities should ensure that hand hygiene supplies are readily available to all personnel in every care location.
- Personal Protective Equipment Training
Employers should select appropriate PPE and provide it to HCP in accordance with OSHA PPE standards (29 CFR 1910 Subpart I). HCP must receive training on and demonstrate an understanding of:- when to use PPE
- what PPE is necessary
- how to properly don, use, and doff PPE in a manner to prevent self-contamination
- how to properly dispose of or disinfect and maintain PPE
- the limitations of PPE.
Any reusable PPE must be properly cleaned, decontaminated, and maintained after and between uses. Facilities should have policies and procedures describing a recommended sequence for safely donning and doffing PPE.
The PPE recommended when caring for a patient with suspected or confirmed COVID-19 includes the following:
- Respirator or Facemask (Cloth face coverings are NOT PPE and should not be worn for the care of patients with suspected or confirmed COVID-19 or other situations where use of a respirator or facemask is recommended.)
- Put on an N95 respirator (or equivalent or higher-level respirator) or facemask (if a respirator is not available) before entry into the patient room or care area, if not already wearing one as part of extended use strategies to optimize PPE supply. Other respirators include other disposable filtering facepiece respirators, powered air purifying respirators (PAPRs), or elastomeric respirators.
- N95 respirators or respirators that offer a higher level of protection should be used instead of a facemask when performing or present for an aerosol generating procedure. See appendix for respirator definition.
- Disposable respirators and facemasks should be removed and discarded after exiting the patient’s room or care area and closing the door unless implementing extended use or reuse. Perform hand hygiene after removing the respirator or facemask.
- If reusable respirators (e.g., powered air-purifying respirators [PAPRs] or elastomeric respirators) are used, they should also be removed after exiting the patient’s room or care area. They must be cleaned and disinfected according to manufacturer’s reprocessing instructions prior to re-use.
- When the supply chain is restored, facilities with a respiratory protection program should return to use of respirators for patients with suspected or confirmed SARS-CoV-2 infection. Those that do not currently have a respiratory protection program, but care for patients with pathogens for which a respirator is recommended, should implement a respiratory protection program.
- Eye Protection
- Put on eye protection (i.e., goggles or a face shield that covers the front and sides of the face) upon entry to the patient room or care area, if not already wearing as part of extended use strategies to optimize PPE supply.
- Protective eyewear (e.g., safety glasses, trauma glasses) with gaps between glasses and the face likely do not protect eyes from all splashes and sprays.
- Ensure that eye protection is compatible with the respirator so there is not interference with proper positioning of the eye protection or with the fit or seal of the respirator.
- Remove eye protection after leaving the patient room or care area, unless implementing extended use.
- Reusable eye protection (e.g., goggles) must be cleaned and disinfected according to manufacturer’s reprocessing instructions prior to re-use. Disposable eye protection should be discarded after use unless following protocols for extended use or reuse.
- Put on eye protection (i.e., goggles or a face shield that covers the front and sides of the face) upon entry to the patient room or care area, if not already wearing as part of extended use strategies to optimize PPE supply.
- Gloves
- Put on clean, non-sterile gloves upon entry into the patient room or care area.
- Change gloves if they become torn or heavily contaminated.
- Remove and discard gloves before leaving the patient room or care area, and immediately perform hand hygiene.
- Put on clean, non-sterile gloves upon entry into the patient room or care area.
- Gowns
- Put on a clean isolation gown upon entry into the patient room or area. Change the gown if it becomes soiled. Remove and discard the gown in a dedicated container for waste or linen before leaving the patient room or care area. Disposable gowns should be discarded after use. Cloth gowns should be laundered after each use.
Facilities should work with their health department and healthcare coalition to address shortages of PPE.
Aerosol Generating Procedures (AGPs)
- Some procedures performed on patients with suspected or confirmed SARS-CoV-2 infection could generate infectious aerosols. Procedures that pose such risk should be performed cautiously and avoided if possible.
- If performed, the following should occur:
- HCP in the room should wear an N95 or equivalent or higher-level respirator, eye protection, gloves, and a gown.
- The number of HCP present during the procedure should be limited to only those essential for patient care and procedure support. Visitors should not be present for the procedure.
- AGPs should ideally take place in an AIIR.
- Clean and disinfect procedure room surfaces promptly as described in the section on environmental infection control below.
Collection of Diagnostic Respiratory Specimens
- When collecting diagnostic respiratory specimens (e.g., nasopharyngeal or nasal swab) from a patient with possible SARS-CoV-2 infection, the following should occur:
- Specimen collection should be performed in a normal examination room with the door closed.
- HCP in the room should wear an N95 or equivalent or higher-level respirator (or facemask if a respirator is not available), eye protection, gloves, and a gown.
- If respirators are not readily available, they should be prioritized for other procedures at higher risk for producing infectious aerosols (e.g., intubation), instead of for collecting diagnostic respiratory specimens. The number of HCP present during the procedure should be limited to only those essential for patient care and procedure support. Visitors should not be present for specimen collection.
- Clean and disinfect procedure room surfaces promptly as described in the section on environmental infection control below.
Manage Visitor Access and Movement Within the Facility
- Limit visitors to the facility to only those essential for the patient’s physical or emotional well-being and care (e.g., care partner, parent).
- Encourage use of alternative mechanisms for patient and visitor interactions such as video-call applications on cell phones or tablets.
- If visitation to patients with SARS-CoV-2 infection occurs, visits should be scheduled and controlled to allow for the following:
- Facilities should evaluate risk to the health of the visitor (e.g., visitor might have underlying illness putting them at higher risk for COVID-19) and ability to comply with precautions.
- Facilities should provide instruction, before visitors enter patients’ rooms, on hand hygiene, limiting surfaces touched, and use of PPE according to current facility policy while in the patient’s room.
- Visitors should not be present during AGPs or other procedures.
- Visitors should be instructed to only visit the patient room. They should not go to other locations in the facility.
Environmental Infection Control
- Dedicated medical equipment should be used when caring for patients with suspected or confirmed SARS-CoV-2 infection.
- All non-dedicated, non-disposable medical equipment used for patient care should be cleaned and disinfected according to manufacturer’s instructions and facility policies.
- Ensure that environmental cleaning and disinfection procedures are followed consistently and correctly.
- Routine cleaning and disinfection procedures (e.g., using cleaners and water to pre-clean surfaces prior to applying an EPA-registered, hospital-grade disinfectant to frequently touched surfaces or objects for appropriate contact times as indicated on the product’s label) are appropriate for SARS-CoV-2 in healthcare settings, including those patient-care areas in which aerosol generating procedures are performed.
- Refer to List N on the EPA website for EPA-registered disinfectants that have qualified under EPA’s emerging viral pathogens program for use against SARS-CoV-2.
- Management of laundry, food service utensils, and medical waste should also be performed in accordance with routine procedures.
- Additional information about recommended practices for terminal cleaning of rooms and PPE to be worn by environmental services personnel is available in the Healthcare Infection Prevention and Control FAQs for COVID-19
Appendix: Additional Information about Airborne Infection Isolation Rooms, Respirators and Facemasks
Information about Airborne Infection Isolation Rooms (AIIRs):
- AIIRs are single-patient rooms at negative pressure relative to the surrounding areas, and with a minimum of 6 air changes per hour (12 air changes per hour are recommended for new construction or renovation).
- Air from these rooms should be exhausted directly to the outside or be filtered through a high-efficiency particulate air (HEPA) filter directly before recirculation.
- Room doors should be kept closed except when entering or leaving the room, and entry and exit should be minimized.
- Facilities should monitor and document the proper negative-pressure function of these rooms.
Information about Respirators:
- A respirator is a personal protective device that is worn on the face, covers at least the nose and mouth, and is used to reduce the wearer’s risk of inhaling hazardous airborne particles (including dust particles and infectious agents), gases, or vapors. Respirators are certified by the CDC/NIOSH, including those intended for use in healthcare.
- Respirator use must be in the context of a complete respiratory protection program in accordance with OSHA Respiratory Protection standard (29 CFR 1910.134). HCP should be medically cleared and fit tested if using respirators with tight-fitting facepieces (e.g., a NIOSH-approved N95 respirator) and trained in the proper use of respirators, safe removal and disposal, and medical contraindications to respirator use.
- NIOSH information about respirators
- OSHA Respiratory Protection eToo
- Strategies for Optimizing the Supply of N-95 Respirators
Filtering Facepiece Respirators (FFR) including N95 Respirators
- A commonly used respirator in healthcare settings is a filtering facepiece respirator (commonly referred to as an N95). FFRs are disposable half facepiece respirators that filter out particles.
- To work properly, FFRs must be worn throughout the period of exposure and be specially fitted for each person who wears one. This is called “fit testing” and is usually done in a workplace where respirators are used.
- Three key factors for an N95 respirator to be effective
- FFR users should also perform a user seal check to ensure proper fit each time an FFR is used.
- Learn more about how to perform a user seal check
- A list of NIOSH-approved FFRs is located on the NIOSH-Approved Particulate Filtering Facepiece Respirators List.
Powered Air Purifying Respirators (PAPRs)
- PAPRs have a battery-powered blower that pulls air through attached filters, canisters, or cartridges. They provide protection against gases, vapors, or particles, when equipped with the appropriate cartridge, canister, or filter.
- Loose-fitting PAPRs do not require fit testing and can be used with facial hair.
- A list of NIOSH-approved PAPRs is located on the NIOSH Certified Equipment List.
Information about Facemasks:
- If worn properly, a facemask helps block respiratory secretions produced by the wearer from contaminating other persons and surfaces (often called source control).
- Surgical facemasks are cleared by the U.S. Food and Drug Administration (FDA) for use as medical devices. Facemasks should be used once and then thrown away in the trash.
Definitions:
Healthcare Personnel (HCP): HCP refers to all paid and unpaid persons serving in healthcare settings who have the potential for direct or indirect exposure to patients or infectious materials, including body substances (e.g., blood, tissue, and specific body fluids); contaminated medical supplies, devices, and equipment; contaminated environmental surfaces; or contaminated air. HCP include, but are not limited to, emergency medical service personnel, nurses, nursing assistants, physicians, technicians, therapists, phlebotomists, pharmacists, students and trainees, contractual staff not employed by the healthcare facility, and persons not directly involved in patient care, but who could be exposed to infectious agents that can be transmitted in the healthcare setting (e.g., clerical, dietary, environmental services, laundry, security, engineering and facilities management, administrative, billing, and volunteer personnel).
Source Control: Use of cloth face coverings or facemasks to cover a person’s mouth and nose to prevent spread of respiratory secretions when they are talking, sneezing, or coughing. Facemasks and cloth face coverings should not be placed on children under age 2, anyone who has trouble breathing, or anyone who is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.
Cloth face covering: Textile (cloth) covers that are intended for source control. They are not personal protective equipment (PPE) and it is uncertain whether cloth face coverings protect the wearer. Guidance on design, use, and maintenance of cloth face coverings is available.
Facemask: Facemasks are PPE and are often referred to as surgical masks or procedure masks. Use facemasks according to product labeling and local, state, and federal requirements. FDA-cleared surgical masks are designed to protect against splashes and sprays and are prioritized for use when such exposures are anticipated, including surgical procedures. Facemasks that are not regulated by FDA, such as some procedure masks, which are typically used for isolation purposes, may not provide protection against splashes and sprays.
Respirator: A respirator is a personal protective device that is worn on the face, covers at least the nose and mouth, and is used to reduce the wearer’s risk of inhaling hazardous airborne particles (including dust particles and infectious agents), gases, or vapors. Respirators are certified by the CDC/NIOSH, including those intended for use in healthcare. Refer to the Appendix for a summary of different types of respirators.
Substantial community transmission: Large scale community transmission, including communal settings (e.g., schools, workplaces)
Minimal to moderate community transmission: Sustained transmission with high likelihood or confirmed exposure within communal settings and potential for rapid increase in cases
No to minimal community transmission: Evidence of isolated cases or limited community transmission, case investigations underway; no evidence of exposure in large communal setting





















.png)












No hay comentarios:
Publicar un comentario