
MTFs plan and prepare to face any emergency or disaster

Staff from Madigan Army Medical Center care for victims of an Amtrak derailment that occurred near Joint Base Lewis-McChord, Washington in December 2017. (Photo Credit: John Wayne Liston, Madigan Army Medical Center.)
For military medical treatment facilities preparing for emergencies and natural disasters, Mark Starnes offers this advice: “Train like you fight.” As the emergency manager at Naval Medical Center Camp Lejeune aboard Marine Corps Base Camp Lejeune in Jacksonville, North Carolina, Starnes and his team begin emergency preparations with routine drills and exercises long before an actual disaster strikes.
“We perform a vulnerability analysis, develop a training plan, have a solid checklist, and prepare for ‘known’ vulnerabilities as early in the season as possible,” said Starnes.
Storm preparations allowed NMCCL staff to continue caring for patients during Hurricane Dorian, a category 2 storm that passed over Eastern North Carolina in September 2019. Contingency measures as part of the medical center’s planning even accounted for the peace of mind of staff, bringing in families and pets of essential personnel during the hurricane. “We think that while on board during an emergency, a person cannot worry about those potentially left at home to evacuate or remain in their house,” Starnes said. “Patients receive better care when the staff is considered a ‘family’ in itself.”
Planning for emergencies is all about mitigation, preparedness, response, and recovery efforts, said Craig Williams, emergency manager at Evans Army Community Hospital at Fort Carson, Colorado. The military base and hospital maintain robust emergency management plans and conduct frequent practice drills and exercises to help build a sense of collaboration. These steps ensure everyone knows what they’re doing in a time of crisis.
In 2018, a fire broke out on the southwest portion of Fort Carson near the hospital and a housing area, resulting in a joint hospital-base response. “We worked closely together, in coordination with local community partners, to ensure everyone’s safety,” Williams said, adding protecting and preventing damage to buildings was also a top priority in their response efforts.
Military hospitals are not an island apart from the civilian community, Starnes added. Collaboration and a unified response to a natural disaster are critical since a community or region will be affected, not just one building.
An Amtrak train derailment near DuPoint, Washington in December 2017, resulted in several passenger cars plunging off an overpass onto the interstate. The staff at Madigan Army Medical Center sprang into action, transporting 19 injured passengers to the hospital. “The proximity of the derailment to Madigan and Joint Base Lewis-McChord facilitated the fastest response times and enabled the most critical casualties to receive lifesaving care more quickly than if they had been transported to local hospitals,” said Bill Llewellyn, Madigan’s senior emergency management coordinator.
As military medical treatment facilities conduct disaster preparations during a global pandemic, Starnes recommends taking COVID-19 patients into account during any emergency. “We have measures in place in coordination with the base to separate COVID-type patients in shelters operated by the Marines with medical oversight and on-station capabilities,” he said. Hospitals should also focus on basics and local needs first. All emergencies are local at one level, he said. A hurricane could result in high wind and road conditions that leave a medical center temporarily isolated. “I definitely want to maintain a well-balanced overall look at all contingencies we may face,” he said.
During Hurricane Dorian, planning for all contingencies included ensuring the safety of high-risk expectant mothers and their immediate families at NMCCL. “A rescue cannot always get to all places in a hurricane or respond to areas in high wind and water,” Starnes said. “Expectant mothers need a little extra attention during a hurricane, and it’s a potential medical emergency we can avoid in advance of a storm.”
Regardless of how great a plan may seem on paper, practice is critical. “Unless the plan is rehearsed and vetted with the military installation and local community partners, there is no assurance that the response will be successful,” said Williams. “Communications, rehearsals, and a realistic response plan are critical to the success of any emergency response.”
The current COVID-19 pandemic can offer valuable lessons on emergency management planning, said Williams. “Be detailed in the planning process, test and evaluate the plan, be flexible, implement changes quickly when necessary, implement improvement plans, reevaluate changes, and update policies and procures for future operations.”
Ultimately, practice drills can’t replicate a real-world disaster that tests plans and assumptions on an entirely different level, added Llewellyn. Post-disaster response evaluation is an important part of emergency planning. After the train derailment in 2017, Madigan revised its policies and procedures based on lessons learned. Leadership created a dedicated emergency operations center with equipment capable of receiving and reporting near real-time situation reports and trained staff accordingly. They also implemented the use of the Incident Command System that provides a common hierarchy of emergency response coordination used by state and local agencies.
“When communication and coordination started moving into JBLM and Madigan, the lines of command and control blurred because Incident Command was unfamiliar causing minor confusion and some delay,” Llewellyn said. “This is a large cultural change for any military organization as it is not a rank-based command and control, but rather training, experience, and job specialty-based.”
Military Health System beneficiaries can also make advance preparations for potential emergencies due to severe weather by visiting TRICARE and signing up for disaster alerts.
MHS asks COVID-19 recovered to donate plasma for seriously ill
Article
8/4/2020

Plasma donations needed in the fight against COVID-19
Air Force mental health team provides for deployed troops
Article
8/4/2020

The Disaster Mental Health team helps combat the stressors of the novel coronavirus and improves the overall well-being of service members of Al Udeid Air Base in Qatar.
DoD leadership updates Pentagon on COVID-19 testing capabilities
Article
8/3/2020

How COVID-19 testing helps prevent spread of the virus
Army Medicine leaders visit BACH’s COVID-19 frontlines
Article
8/3/2020

The commander shared both successes and challenges in the face of a global pandemic.
Air Force medical technician drawn to caring for others
Article
7/31/2020

"As a medic, my job is to test people for the virus to help make sure they’re safe."
In this Together: Military Couple Recovers from COVID-19, Donates Convalescent Plasma
Article
7/30/2020
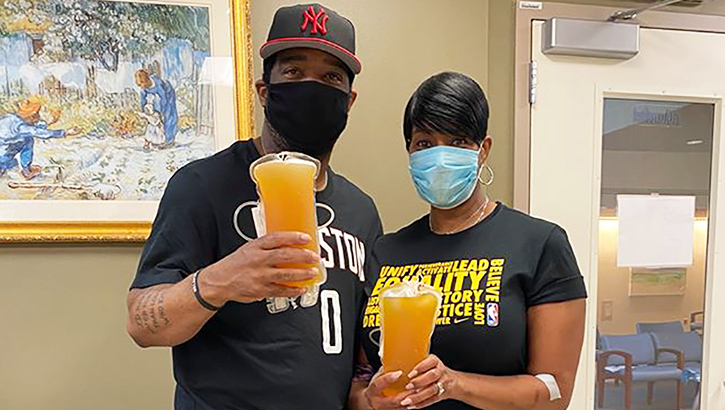
There is information that suggests CCP might help some patients recover from the disease.
Military Health System experts discuss COVID-19 innovations
Article
7/30/2020

How quick thinking and new approaches are saving lives in the pandemic fight.
DoD COVID-19 Practice Management Guide Version 5
Technical Document
7/30/2020
This Practice Management Guide does not supersede DoD Policy. It is based upon the best information available at the time of publication. It is designed to provide information and assist decision making. It is not intended to define a standard of care and should not be construed as one. Neither should it be interpreted as prescribing an exclusive course of management. It was developed by experts in this field. Variations in practice will inevitably and appropriately occur when clinicians take into account the needs of individual patients, available resources, and limitations unique to an institution or type of practice. Every healthcare professional making use of this guideline is responsible for evaluating the appropriateness of applying it in the setting of any particular clinical situation. The Practice Management Guide is not intended to represent TRICARE policy. Further, inclusion of recommendations for specific testing and/or therapeutic interventions within this guide does not guarantee coverage of civilian sector care. Additional information on current TRICARE benefits may be found at www.tricare.mil or by contacting your regional TRICARE Managed Care Support Contractor.
McCaffery offers HA perspective to COVID-19
Article
7/29/2020

How a whole-government effort aided in pandemic response
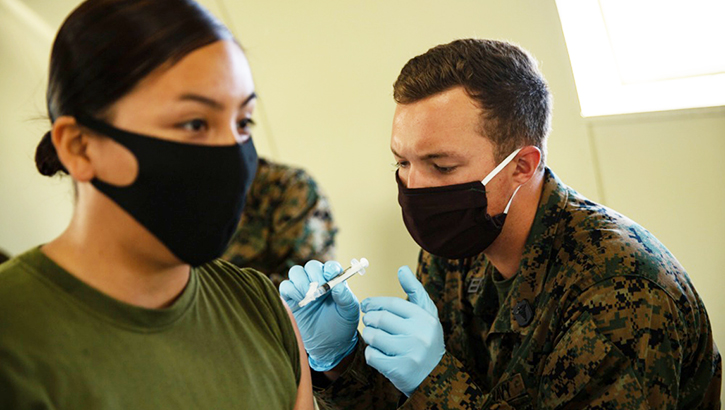
Marines donate plasma in fight against COVID-19
Article
7/29/2020
All of the Marines volunteered to donate their plasma with the hope that their antibodies will help others.
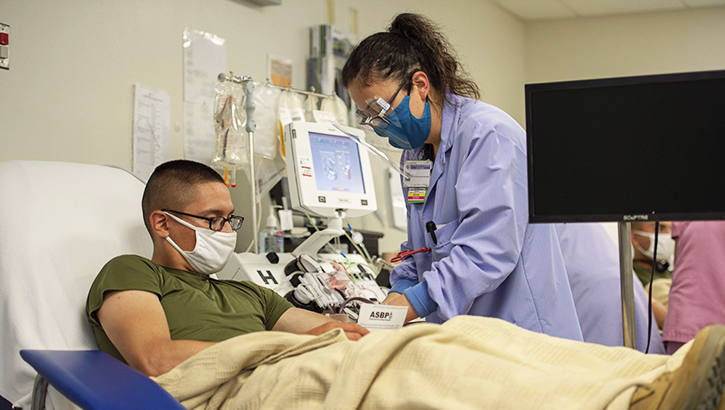
Bliss blood program faces supply shortage; begins testing for coronavirus antibodies
Article
7/27/2020

[A]ntibodies do not indicate immunity from the virus; it simply means the patient was exposed to it.
USS Nimitz certified to administer CCP
Article
7/24/2020

Navy carrier crews take care of their shipmates.
MHS emphasizes importance of vaccinations
Article
7/22/2020
Get questions answered during live Q&A on July 23
Determined to Serve: Critical care nurse joins the Reserve at age 50
Article
7/22/2020

The Air Force Reserve does indeed have a critical need for critical care nurses.
Defending the Homeland: NMRTC Bremerton ensures Operational Readiness and a Medically Ready Force
Article
7/22/2020

Supporting mission readiness has long been a responsibility for the ready medical force of NMRTC Bremerton.





















.png)












No hay comentarios:
Publicar un comentario