
Interim Guidelines for COVID-19 Antibody Testing
Data to inform antibody testing (also referred to as serologic testing) guidance is rapidly evolving. Recommendations on the use of serologic tests to determine protective immunity and infectiousness among persons recently infected with SARS-CoV-2 will be updated as new information becomes available.
Interim Guidelines for COVID-19 Antibody Testing
Interim Guidelines for COVID-19 Antibody Testing in Clinical and Public Health Settings
Data that will inform antibody testing (also referred to as serologic testing) guidance are rapidly evolving. Recommendations on the use of serologic tests to determine protective immunity and infectiousness among persons recently infected with SARS-CoV-2 will be updated as new information becomes available.
Summary
On This Page
Serologic methods have important public health and clinical uses for monitoring and responding to the COVID-19 pandemic.
- Several serologic assays for SARS-CoV-2 have Emergency Use Authorization (EUA) by the U.S. Food and Drug Administration (FDA), which has independently reviewed their performance.
- Currently, there is no identified advantage whether the assays test for IgG, IgM and IgG, or total antibody.
- It is important to minimize false-positive test results by choosing an assay with high specificity and by testing populations and individuals with an elevated likelihood of previous exposure to SARS-CoV-2. Alternatively, an orthogonal testing algorithm (i.e., employing two independent tests in sequence when the first test yields a positive result) can be used when the expected positive predictive value of a single test is low.
- Antibodies most commonly become detectable 1–3 weeks after symptom onset, at which time evidence suggests that infectiousness likely is greatly decreased and that some degree of immunity from future infection has developed. However, additional data are needed before modifying public health recommendations based on serologic test results, including decisions on discontinuing physical distancing and using personal protective equipment.
Background
Serologic assays for SARS-CoV-2, now broadly available, can play an important role in understanding the virus’s epidemiology in the general population and identifying groups at higher risk for infection. Unlike direct detection methods such as viral nucleic acid amplification or antigen detection tests that can detect acutely infected persons, antibody tests help determine whether the individual being tested was previously infected—even if that person never showed symptoms. Serologic tests detect resolving or past SARS-CoV-2 virus infection indirectly by measuring the person’s humoral immune response to the virus. Therefore, serologic assays do not typically replace direct detection methods as the primary tool for diagnosing an active SARS-CoV-2 infection, but they do have several important applications in monitoring and responding to the COVID-19 pandemic.
Although serologic tests should not be used at this time to determine if an individual is immune, these tests can help determine the proportion of a population previously infected with SARS-CoV-2 and provide information about populations that may be immune and potentially protected. Thus, demographic and geographic patterns of serologic test results can help determine which communities may have experienced a higher infection rate and therefore may have a higher proportion of the population with some degree of immunity, at least temporarily. In some instances, serologic test results may assist with identifying persons potentially infected with SARS-CoV-2 and determining who may qualify to donate blood that can be used to manufacture convalescent plasma as a possible treatment for those who are seriously ill from COVID-19.
Development of Antibodies and Immunity
Nearly all immune-competent individuals will develop an immune response following SARS-CoV-2 infection. Like infections with other pathogens, SARS-CoV-2 infection elicits development of IgM and IgG antibodies, which are the most useful for assessing antibody response because little is known about IgA response in the blood.
Antibodies in some persons can be detected within the first week of illness onset. In SARS-CoV-2 infections, IgM and IgG antibodies can arise nearly simultaneously in serum within 2 to 3 weeks after illness onset. Thus, detection of IgM without IgG is uncommon. How long IgM and IgG antibodies remain detectable following infection is not known. It is also important to note that some persons do not develop detectable IgG or IgM antibodies following infection. Thus, the absence of detectable IgM or IgG antibodies does not necessarily rule out that they could have previously been infected.
In addition, development of neutralizing antibodies can also be assessed. Neutralizing antibodies inhibit viral replication in vitro, and as with many infectious diseases, their presence correlates with immunity to future infection, at least temporarily.
Recurrence of COVID-19 illness appears to be very uncommon, suggesting that the presence of antibodies could indicate at least short-term immunity to infection with SARS-CoV-2. Consistent with this observation, experimental primary infection in primates and subsequent development of antibodies resulted in protection from reinfection after the primates were rechallenged. Additionally, antibody development in humans correlates with a marked decrease in viral load in the respiratory tract. Taken together, these observations suggest that the presence of antibodies may decrease a person’s infectiousness and offer some level of protection from reinfection. However, it remains uncertain to what degree and for how long individuals with antibodies (neutralizing or total) are protected against reinfection with SARS-CoV-2 or what concentration of antibodies may be needed to provide such protection.
Current Status of Antibody Testing in the United States
Antigenic targets
The two major antigenic targets of SARS-CoV-2 virus against which antibodies are detected are spike glycoprotein (S) and nucleocapsid phosphoprotein (N). While S protein is essential for virus entry and is present on the viral surface, N protein is the most abundantly expressed immunodominant protein that interacts with RNA. Multiple forms of S protein—full-length (S1+S2) or partial (S1 domain or receptor binding domain [RBD])—are used as antigens. The protein target determines cross-reactivity and specificity because N is more conserved across coronaviruses than S, and within S, RBD is more conserved than S1 or full-length S.
Types of Antibody Testing
Different types of assays can be used to determine different aspects of immune response and functionality of antibodies. The tests can be broadly classified to detect either binding or neutralizing antibodies.
- Binding antibody detection: These tests use purified proteins of SARS-CoV-2, not live virus, and can be performed in lower biosafety level laboratories (e.g., BSL-2). With specific reagents, individual antibody types, like IgG, IgM, and IgA, can be determined. Although scientists do not know how long antibodies to SARS-CoV-2 can be detected, for most other infections, IgM is most useful for determining recent infection as it usually becomes undetectable weeks to months following infection, while IgG may remain detectable for months or years. IgA is important for mucosal immunity and can be detected in mucous secretions like saliva in addition to blood, though its significance in this disease is still to be determined. Depending on the complexity of assays, these tests can be performed rapidly (in less than 30 minutes) in a field setting or in a few hours in a laboratory.Tests that detect binding antibodies fall into two broad categories.
- Point-of-care (POC) tests generally are lateral flow devices that detect IgG, IgG and IgM, or total antibody in serum, plasma, whole blood, and/or saliva. An advantage of some point-of-care tests using whole blood is that they can be performed on blood samples obtained by fingerstick rather than venipuncture.
- Laboratory tests use ELISA (enzyme-linked immunosorbent assay) or CIA (chemiluminescent immunoassay) methods for antibody detection, which for some assays may require trained laboratorians and specialized instruments. Based on the reagents, IgG, IgM, and IgA can be detected separately or combined as total antibody.
Surrogate virus neutralization tests (sVNT) have also been developed. These are binding antibody tests designed to detect potential neutralizing antibodies, often those that prevent interaction of RBD with angiotensin-converting enzyme 2 (ACE2, the cell surface receptor for SARS-CoV-2). Because these tests do not require live virus, they can be conducted in BSL-2 laboratories.
- Neutralizing antibody detection: FDA has not yet authorized the use of neutralization tests for SARS-CoV-2. Neutralization tests determine the functional ability of antibodies to prevent infection of virus in vitro. The tests involve incubating serum or plasma with live virus followed by infection and incubation of cells. Testing will require either BSL-3 or BSL-2 laboratories, depending on what form of the SARS-CoV-2 virus is used.Two types of neutralization tests are conducted.
- Virus neutralization tests (VNT), such as the plaque-reduction neutralization test (PRNT) and microneutralization, use a SARS-CoV-2 virus from a clinical isolate or recombinant SARS-CoV-2 expressing reporter proteins. This testing requires BSL-3 laboratories and may take up to 5 days to complete.
- Pseudovirus neutralization tests (pVNT) use recombinant pseudoviruses (like vesicular stomatitis virus, VSV) that incorporate the S protein of SARS-CoV-2. This testing can be performed in BSL-2 laboratories depending on the VSV strain used.
FDA-authorized serologic tests
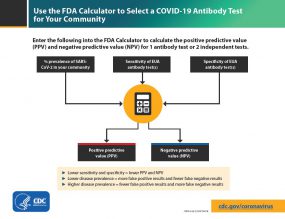
Use the FDA Calculator to select a COVID-19 Antibody Test for your community.
FDA now requires commercially marketed serologic tests to receive Emergency Use Authorization (EUA). Tests that are not commercially marketed do not require FDA authorization, but developers may voluntarily request authorization. Multiple agencies—including FDA, the National Cancer Institute/National Institutes of Health (NCI/NIH), CDC, and the Biomedical Advanced Research and Development Authority (BARDA)—are collaborating with members of academia and the medical community to evaluate several serology tests using a well-characterized set of clinical samples (serum or plasma) collected before and during the current COVID-19 outbreak. A list of all tests authorized for emergency use under EUA is maintained on an FDA website. All currently authorized tests are qualitative (providing a result that is positive, negative, or indeterminate) rather than quantitative (providing a quantitative assessment of antibody levels).
Both laboratory and rapid serologic assays have received EUA. Serologic testing technologies include single-use, low-throughput lateral flow tests where the presence of antibody is demonstrated by a color change on a paper strip and laboratory-based immunoassays that allow for processing of many samples at the same time.
The EUA letter of authorization includes the settings in which the test is authorized, based on FDA’s determination of appropriate settings for use during the public health emergency.
Optimizing Testing Outcomes
Test performance
The utility of tests depends on the sensitivity and specificity of the assays; these performance characteristics are determined by using a defined set of negative and positive samples. In addition, the predictive values of a test should be considered because these values affect the overall outcome of testing. Positive predictive value is the probability that individuals with positive test results are truly antibody positive. Negative predictive value is the probability that individuals with negative test results are truly antibody negative. Positive and negative predictive values are determined by the percentage of truly antibody positive individuals in the tested population (prevalence, pre-test probability) and the sensitivity and specificity of the test. For example:
- In a high-prevalence setting, the positive predictive value increases—meaning it is more likely that persons who test positive are truly antibody positive—than if the test is performed in a population with low prevalence. When a test is used in a population where prevalence is low, the positive predictive value drops because there are more false-positive results, since the pre-test probability is low.
- Likewise, negative predictive value is also affected by prevalence. In a high-prevalence setting, the negative predictive value declines whereas in a low-prevalence setting, it increases.
In most of the country, including areas that have been heavily impacted by COVID-19, the prevalence of SARS-CoV-2 antibody is expected to be low, ranging from <5% to 25%, so that testing at this point might result in relatively more false-positive results and fewer false-negative results.
In some settings, such as COVID-19 outbreaks in food processing plants and congregate living facilities, the prevalence of infection in the population may be significantly higher. In such settings, serologic testing at appropriate intervals following outbreaks might result in relatively fewer false-positive results and more false-negative results.
Testing strategies
In the current pandemic, maximizing specificity and thus positive predictive value in a serologic algorithm is preferred in most instances, since the overall prevalence of antibodies in most populations is likely low. For example, in a population where the prevalence is 5%, a test with 90% sensitivity and 95% specificity will yield a positive predictive value of 49%. In other words, less than half of those testing positive will truly have antibodies. Alternatively, the same test in a population with an antibody prevalence exceeding 52% will yield a positive predictive value greater than 95%, meaning that fewer than one in 20 people testing positive will have a false-positive test result.
Three strategies can be used to improve positive predictive value:
- Choosing a test with a very high specificity, perhaps 99.5% or greater, will yield a high positive predictive value in populations tested with low prevalence; however, the positive predictive value will show some variation based on the population prevalence with a single test strategy. Table 1 presents the positive predictive value for hypothetical populations with various SARS-CoV-2 antibody prevalences using a test with 90% sensitivity and 99.8% specificity.
- Another strategy is to focus testing on persons with a high pre-test probability of having SARS-CoV-2 antibodies, such as persons with a history of COVID-19-like illness.
- A third approach is to employ an orthogonal testing algorithm in which persons who initially test positive are tested with a second test. Effective orthogonal algorithms are generally based on testing a patient sample with two tests, each with unique design characteristics (e.g., antigens or formats).
Several tests are available with specificities of 99.5% or greater. Because specificity may vary according to the panel of specimens collected, FDA, NIH, and CDC have conducted an independent evaluation of some tests using a standard panel of specimens. Specificities of at least 99.5% are required to achieve a high positive predictive value in low-prevalence populations (Table 1). Tests with lower specificity, for example a specificity of 95%, will result in suboptimal positive predictive values when used in low-prevalence populations. In this situation, orthogonal testing algorithms can be designed to maximize overall specificity while retaining maximum sensitivity.
The performance of orthogonal testing algorithms has not been systematically evaluated but can be estimated using an online calculator from FDA. See Table 2 for the potential improvement benefits of the orthogonal testing algorithm. The type of antigen and the Ig class of both tests in an orthogonal testing algorithm should be considered when interpreting test results. For example, a person infected with SARS-CoV-2 may develop an immune response that is heavily biased towards a particular viral protein (e.g., spike protein). This scenario may result in discordant test results if the detection antigens in the first and second tests were spike protein and nucleoprotein, respectively. Similarly, the temporal dynamics of virus-specific IgM and IgG immune responses may differ following infection. In this scenario, using tests that detect different Ig classes (total Ig, IgM or IgG) may lead to discordant results.
Limitations of Serologic Tests
At present, the immunologic correlates of immunity from SARS-CoV-2 infection are not well defined. Representatives from BARDA, CDC, FDA, NIH, the Office of the Assistant Secretary for Health (OASH), Department of Defense (DoD), and White House Office of Science and Technology Policy (OSTP) are working with members of academia and the medical community to determine whether positive serologic tests are indicative of protective immunity against SARS-CoV-2. This work includes assessing the level of antibodies required for protection from reinfection, the duration of that protection, and the factors associated with development of a protective antibody response. The kinetics of antibody response, longevity of antibodies, the ability of antibodies to protect from repeat infection, the protective titer of neutralizing antibody, and the correlation of binding antibody titers to neutralization ability are yet to be determined. Although animal challenge studies demonstrate protection in the short run, demonstration of long-term protection in humans will require future study. Hence, pending additional data, the presence of antibodies cannot be equated with an individual’s immunity from SARS-CoV-2 infection.
Some tests may exhibit cross-reactivity with other coronaviruses, such as those that cause the common cold. This could result in false-positive test results. Some persons may not develop detectable antibodies after coronavirus infection. In others, it is possible that antibody levels could wane over time to undetectable levels. IgM and IgG antibodies may take 1 to 3 weeks to develop after infection. Thus, serologic test results do not indicate with certainty the presence or absence of current or previous infection with SARS-CoV-2.
Recommendations for Use of Serologic Tests
Information that might impact serologic recommendations is rapidly evolving, particularly evidence of whether positive serologic tests indicate protective immunity or decreased transmissibility among those recently ill. These recommendations will be updated as new information becomes available.
Choice of test and testing strategy
- Serologic assays that have Emergency Use Authorization (EUA) are preferred for public health or clinical use since their test performance data have been reviewed by FDA.
- Serologic test results should be interpreted in the context of the expected predictive values, positive and negative.
- Positive predictive value should be optimized, particularly if results are returned to individuals, in the following ways:
- Assure a high positive predictive value (e.g., 95%) by choosing tests with sufficiently high specificity (e.g., > 99.5%) and testing persons or populations with a high pre-test probability of having antibodies (e.g., persons with a history of symptoms compatible with COVID-19 or who are exposed to areas or institutions experiencing outbreaks), OR
- If a high positive predictive value cannot be assured with a single test, use an orthogonal testing algorithm. See Table 2 for examples of using one or two tests in populations with various prevalences of SARS-CoV-2 antibodies.
- Currently, there is no substantive performance advantage of assays whether they test for IgG, IgM and IgG, or total antibody. Thus, immunoglobulin class should not determine the assay chosen in most circumstances. The detection of IgM antibodies may indicate a more recent infection, but the dynamics of the IgM antibody response are not well defined at present. Over time, it may be important to characterize and evaluate the performance of assays in samples that are IgM negative and IgG positive to ensure that assays remain fit for purpose in population studies as the pandemic progresses and more individuals are expected to have lower IgM levels.
- Serologic testing should not be used to determine immune status in individuals until the presence, durability, and duration of immunity are established.
- Serologic testing can be offered as a method to support diagnosis of acute COVID-19 illness for persons who present late.* For persons who present 9–14 days after illness onset, serologic testing can be offered in addition to recommended viral direct detection methods such as polymerase chain reaction or antigen detection tests. During this time period, the sensitivity of nucleic acid detection is decreasing, and the sensitivity of serologic testing is increasing.
- Serologic testing should be offered as a method to help support a diagnosis when patients present with late complications of COVID-19 illness, such as multisystem inflammatory syndrome in children.
- Serologic testing by itself should not be used to establish the presence or absence of SARS-CoV-2 infection or reinfection. Antibodies may not be present among those tested early in illness before antibodies develop or among those who never develop detectable antibodies following infection. In addition, the presence of antibodies may reflect previous infection and may be unrelated to the current illness.
Recommendations for persons who test positive for anti-SARS-CoV-2 antibodies
- The presence of anti-SARS-CoV-2 antibodies indicates a previous infection and possibly at least some degree of immunity or protection against future SARS-CoV-2 infection. However, until the durability and duration of immunity are established, it cannot be assumed that individuals who test positive for SARS-CoV-2 antibodies, including total antibody, IgM, IgG, or IgA, are protected from future infection.
- Asymptomatic persons who test positive by serologic testing without recent history of a COVID-19 confirmed or compatible illness have a low likelihood of active infection and should follow general recommendations to prevent infection with SARS-CoV-2. They should continue with normal activities, including work.
- Persons who have had a COVID-19 compatible or confirmed illness should follow previous guidance regarding when to resume normal activities, including work, regardless of the presence of antibodies.
- There should be no change in clinical practice or use of personal protective equipment (PPE) by health care workers and first responders who test positive for SARS-CoV-2 antibody.
Additional considerations on the use of serologic tests
- Serologic test results should not be used to make decisions about grouping persons residing in or being admitted to congregate settings, such as schools, dormitories, or correctional facilities.
- Serologic test results should not be used to make decisions about returning persons to the workplace.
- Until more information is available about the dynamics of IgA detection in serum, testing for IgA antibodies is not recommended.
* Detection of specific antibody in serum, plasma, or whole blood that indicates new or recent infection provides presumptive laboratory evidence of COVID-19 illness according to the Council of State and Territorial Epidemiologists (CSTE) interim case definition for COVID-19.
Additional Resources
- American Medical Association. Serological Testing for SARS-CoV-2 Antibodies.
- Infectious Diseases Society of America. IDSA COVID19 Antibody Testing Primer.
- Association of Public Health Laboratories and Council of State and Territorial Epidemiologists. Public Health Considerations: Serologic Testing for COVID-19. Version 1-May 7, 2020.
| Prevalence of COVID-19 in the population | PPV for one test (SE=90%, SP=99.8%) |
|---|---|
| 2% | 90.2% |
| 5% | 95.9% |
| 10% | 98.0% |
| 30% | 99.5% |
PPV = positive predictive value
SE = sensitivity
SP = specificity
| Prevalence of COVID-19 in the population | PPV for one test (SE=90%, SP=95%) | PPV for two orthogonal tests (SE=90%, SP=95%) |
|---|---|---|
| 2% | 26.9% | 86.9% |
| 5% | 48.6% | 94.5% |
| 10% | 66.7% | 97.3% |
| 30% | 88.5% | 99.3% |
PPV = positive predictive value
SE = sensitivity
SP = specificity





















.png)












No hay comentarios:
Publicar un comentario