
Award-winning Navy team successfully improves care for women, infants

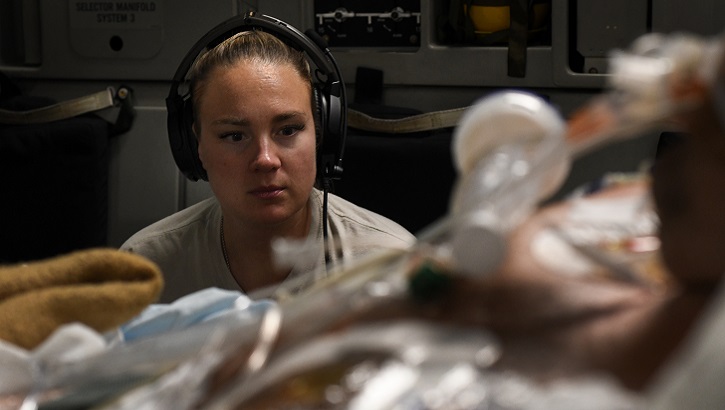
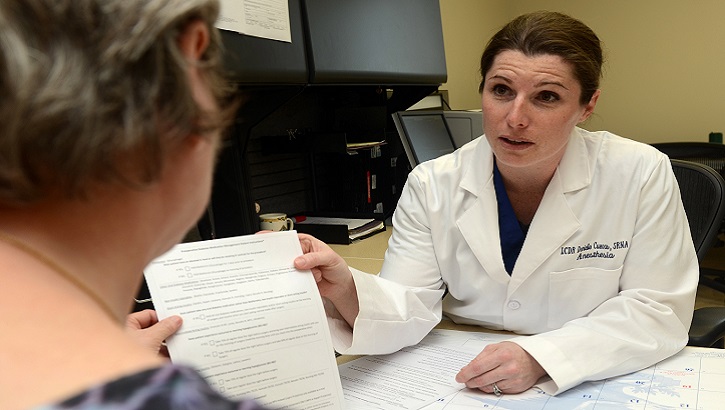
Labor and Delivery providers were the front-line adopters of the Induction of Labor care pathway at Naval Medical Center San Diego. As of July 2019, over 80 percent of the hospital’s providers were using the pathway. (U.S. Navy photo by Mass Communication Specialist Seaman Joseph A. Boomhower)
A team of nurses and providers at Naval Medical Center San Diego were awarded the Rear Adm. Elizabeth S. Niemyer Award for Evidence-Based Practice this August, for their work improving outcomes for pregnant women and babies.
In 2018, childbirth made up 42 percent of all hospital admissions in the MHS. As with other national health systems, data have shown that delivering top outcomes for pregnant women and babies continues to be one of the MHS’s greatest challenges.
This is why providers and staff across the MHS have been working on ways to improve outcomes for pregnant women and babies. The award-winning team at Naval Medical Center San Diego have had some success.
They focused on the care process for inducing labor in pregnant women. In 20 percent of pregnancies, labor must be induced. This can be a long and complex process for mothers and babies. Induction of labor can lead to complications as well. So, the team developed and implemented a care pathway.
Care pathways approach care from the patient’s perspective. They guide a patient with a specific condition through each step of the care experience. Providers use the pathway to ensure all patients receive consistent, high-quality care aligned to best practices.
When the Induction of Labor care pathway was used in the hospital, the team found that patient outcomes improved.
The team saw a 2 percent decrease in unplanned NICU admissions. Time from hospital admission to delivery decreased by an average of four hours. And chorioamnionitis infections in labor went down 5 percent. Chorioamnionitis is a bacterial infection that can affect both mothers and babies.
Now that the team has seen results in San Diego, there may be opportunity to expand and improve outcomes for women and babies across the MHS.
“We are looking for the best way to roll out the pathway to other military treatment facilities,” said the project team lead, Navy Cmdr. (Dr.) Monica Lutgendorf.
This project is just one example of teams improving care for MHS patients. Lutgendorf is the chair of the MHS Women and Infant Clinical Community. The MHS Clinical Communities are networks of MHS providers who collaborate on clinical process improvement and standardization to ensure a consistent level of excellence in patient care at each facility.
“Our Clinical Communities identify, develop and pilot clinical performance improvement projects like the Induction of Labor care pathway to improve the way we deliver care,” said Dr. Paul Cordts, Chief Medical Officer for the Defense Health Agency.
Success in San Diego
The Induction of Labor care pathway was modeled after evidence-based processes used in other health systems. The MHS Women and Infant Clinical Community and the team in San Diego adapted these processes to fit the needs of their patients.
Developing the care pathway was just one step to success. After that, the team had to ensure providers used the pathway, and had to monitor progress for patients. The project team said educating staff, building support and adjusting the pathway were essential to success.
“Cmdr. Lutgendorf’s most critical role was as the provider,” said Jeffrey Budge. Budge is a registered nurse and process improvement expert on the project team. “She led the change and led other providers to adopt the care pathway. Without someone actually using the pathway when taking care of the patients, it’s all theoretical.”
By July 2019, more than 80 percent of the hospital’s providers were using the pathway.
Real-time data collection served an important role in showing the success of the pathway. This helped the team gain the support of other providers. This data will also inform the MHS approach to expanding the pathway to other facilities.
Standardization across the MHS
The MHS Clinical Communities, including the Women and Infant Clinical Community, develop and spread improvements like this pathway. The communities target areas of varying care and apply standard approaches to get the best outcomes for patients.
Current changes within the MHS support standardized and improved care. The Defense Health Agency is becoming responsible for the Army, Navy and Air Force hospitals and clinics. This authority advances the MHS’s efforts to become a reliable system that drives improvement and decreases disparity in care. This will ensure every patient receives the best possible care.
“There is definitely work involved in implementing, but it is rewarding to change the system, and even more rewarding to improve outcomes for your patients,” said Lutgendorf.
Keesler Medical Center receives national recognition
Article
11/27/2019

The ACS National Surgical Quality Improvement Program recognized Keesler Medical Center
Lending a helping, healing hand
Article
11/20/2019

Army nurse supports Navy hospital
Artificial intelligence makes its way to dermatology clinic
Article
11/18/2019

The software was able to correctly identify 95% of malignant skin tumors
Nellis medical center celebrates 25 years
Article
11/13/2019

The Mike O’Callaghan Military Medical Center celebrated 25 years of operation Nov. 12
Womack Army Medical Center named Level III trauma center
Article
11/12/2019

Trauma is the leading cause of death for Americans age 45 and younger
Air Force transitions all U.S. military treatment facilities to DHA administration, management
Article
10/31/2019
Congress directed this transfer in the fiscal year 2017 National Defense Authorization Act
Joint Army-Air Force-Navy medical partnership saves lives downrange
Article
10/29/2019

More than 100 medics from the 59th Medical Wing deployed
DHA's management of hospitals and clinics 'all about the patient'
Article
10/29/2019

Great outcomes, a ready medical force, satisfied patients
State of the art procedure is the first within DoD
Article
10/28/2019

Only a handful of medical centers in the United States perform this surgery
Continuing Implementation of the Reform of the Military Health System
Policy
This memorandum directs the continued implementation of the Military Health System (MHS) organizational reform required by 10 U.S.C. § 1073c, and sections 71 land 712 of the John S. McCain National Defense Authorization Act (NDAA) for Fiscal Year (FY) 2019. The DoD policy for this reform is guided by the goals of improved readiness, better health, better care, and lower cost. The Department will advance these objectives through specific organizational reforms directed by Congress and the continued direction of the Secretary of Defense·anct the National Defense Strategy.
- Identification #: N/A
- Date: 10/25/2019
- Type: Memorandums
- Topics: Military Hospitals and Clinics | MHS Transformation
No effort spared to bring home seriously wounded Soldier
Article
10/17/2019
The priority the military places on saving the lives of its service members is unparalleled
TRICARE website expands to include military hospital sites
Article
10/16/2019
By 2021, more than 350 individual military hospital and clinic websites will move to TRICARE.mil.
For a good grade on bone health, aim for D – vitamin D
Article
10/15/2019

Women generally more deficient than men in this essential nutrient, studies find
Soldier self-amputates leg to aid battle buddies
Article
10/9/2019

If I didn't help myself, my crew, no one was going to
Inclusion of Women and Minorities in the CDMRP
Congressional Testimony
10/7/2019
S. 3159 SAC Report for FY 2019, 115-290 Pg. 213-214


































No hay comentarios:
Publicar un comentario