
Medical team saves newborn’s life

Maria Ortiz, registered nurse, Labor and Delivery Section, William Beaumont Army Medical Center, checks vitals on Vanessa Torres, a laboring mom, as part of daily operations at WBAMC’s L&D section. Recently, Ortiz and other staff members quickly responded to an umbilical cord prolapse, an obstetrical emergency, at WBAMC resulting in the successful delivery of a baby, despite the life-threatening complication. (U.S. Army photo)
For most women, pregnancy is an incredible 40-week journey ending with the delivery of baby. But it’s not always that easy or predictable with possible complications threatening the health of mother, baby or both.
Recently, medical professionals at William Beaumont Army Medical Center’s Labor and Delivery section skillfully dealt with a rare complication when a laboring mom experienced an umbilical cord prolapse, leading staff to quickly respond to the obstetrical emergency via an emergency cesarean section.
A cord prolapse occurs when the umbilical cord prolapses, or drops, through the open cervix into the vagina ahead of the baby which may block fetal-placental circulation resulting in loss of oxygen to the fetus and possible stillbirth if not treated immediately.
“(The patient) was already here and admitted because we were inducing labor,” said Diana Ortiz, charge nurse during the shift of the incident. “The doctor went in there to (rupture) the membrane and the cord came out, he was trying to make her go into labor.”
Although the artificial rupture of membranes is a common procedure performed to accelerate or induce labor, there are always risks involved. According to studies by the Cleveland Clinic, about one in every 500 pregnancies may result in an umbilical cord prolapse, increasing the importance of staff readiness.
“Rupturing of the amniotic sack is just part of the process to help a mom who’s not going into labor any other way, and there are risks associated with that,” said Army Maj. Michael Swift, the obstetrician-gynecologist performing the procedure.
Obstetrical emergencies, such as cord prolapse, are routinely simulated at WBAMC’s L&D section through the use of medical manikins to evaluate staff communication during emergencies, and improve interdisciplinary and clinical performance.
“We do practice simulations but this was beyond simulations, it was just a really, really, solid team,” said Swift. “It was fast, it was extremely fast. Everyone was well organized it was like an absolute perfect orchestra.”
According to the staff, as Swift called for assistance after the prolapse, a team of nurses quickly prepared the operating room for the emergency cesarean section, while another nurse jumped on the gurney with the patient to assist with alleviating pressure on the umbilical cord due to the baby dropping.
“The teamwork was dynamic, and worked out so well,” said Ortiz, a seven-year L&D nursing veteran. “Everybody ran and did something, it synchronized really well, and right at change of shift.”
According to Ortiz, shift changes are usually a more chaotic time during care as outgoing staff are occupied with the transfer of patient information to incoming staff and other activities.
“I’m still catching my breath because everything just fell into place from (umbilical cord prolapse) to (emergency cesarean section),” said Ortiz.
For Swift, who is only two years out of his medical residency, the only other real-world experience with an umbilical cord prolapse was during his residency. He credits the team of nurses for their quick reaction, turning a potentially fatal situation to an otherwise successful delivery.
“These nurses are extremely experienced and have been doing this for years, but it does demonstrate the importance of simulations, because these are practiced routinely,” said swift.
As a result of their actions, staff members were presented commander’s coins following the incident. Staff members include: Santa Ware, Maria Martell, Lisa Obermeyer, Yesenia Ruelas and Jennifer Ruelas.
Within six minutes, the team’s actions went from the umbilical cord prolapse to delivery of the baby with no further complications. Two weeks following discharge, during a follow up appointment the family were content and thankful for the rapid response and teamwork at WBAMC.
“There’s always great crew work, if something happens everybody knows what to do,” said Ortiz.
Disclaimer: Re-published content may have been edited for length and clarity. Read original post.
'Fused' technologies give 3D view of prostate during biopsy
Article
1/9/2019

Other than skin cancer, prostate cancer is the most common cancer in American men
CJTH continues to provide superior care for U.S., coalition forces
Article
1/7/2019

With a 99.3-percent survival rate, the hospital staff have reason to be proud
Langley surgical team goes 'purple'
Article
1/3/2019

A joint surgical team was organized to perform a functional endoscopic sinus surgery
Army hospital earns reputation as a top teaching institution
Article
1/2/2019

CRDAMC has been recognized by healthcare associations and educational institutions for exceptional achievements
Navy corpsman: Carrying the legacy
Article
12/27/2018

Navy hospital corpsmen attend 14-week “A” school at the Medical Education and Training Campus in Joint Base San Antonio — Fort Sam Houston, Texas
Oak Harbor achieves first with crucial new information technology milestone
Article
12/21/2018
Reducing risks to patients’ information is a top priority for the DoD
Hospital ship USNS Comfort returns home after completing mission
Article
12/20/2018

This mission marked the sixth time the hospital ship has provided medical assistance in the region
Surgeons share secrets of residency success
Article
12/11/2018

Madigan's general surgery residents have passed the exam for board certification on their first attempt at a nation-topping rate of 97.6 percent
Fleet surgical team saves life aboard USS Somerset
Article
12/6/2018

We were able to determine he had acute appendicitis
USNS Comfort conducts mass casualty training exercise
Article
10/15/2018

A mass casualty event, by nature, is chaotic
A 'Pharmacy Phamily' team effort recognized at Naval Hospital Bremerton
Article
10/3/2018

Naval Hospital Bremerton’s pharmacy selected for the 2018 Navy Pharmacy Team Award
Robotics key to medical Airmen recruitment, retention, readiness
Article
10/2/2018
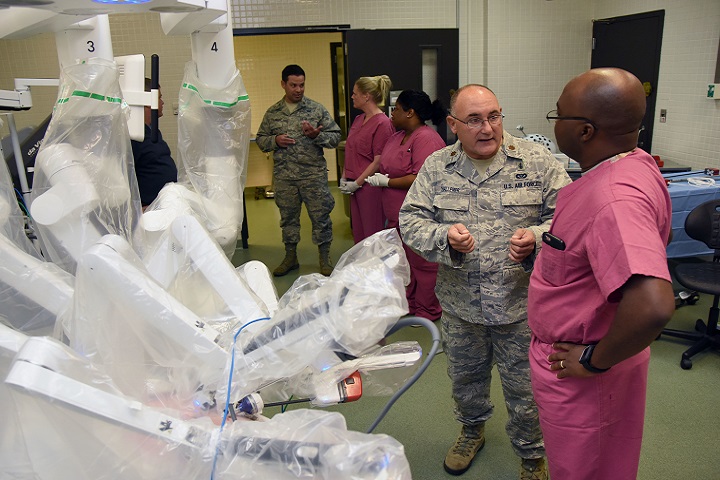
Robotics has been the standard for years in the private sector
DHA assumes management, administration of KMC
Article
10/2/2018

The Keesler Medical Center is the first hospital in the Air Force to transition
Air Force begins transition of hospitals, clinics to the Defense Health Agency
Article
10/2/2018
From a patient perspective, most of these changes should go unnoticed
Implementing Congressional Direction for Reform of the Military Health System
Policy
Policy Memorandum, signed by Deputy Secretary of Defense Patrick M. Shanahan, to direct implementation of the Military Health System (MHS) organizational reform required by the National Defense Authorization Act.


































No hay comentarios:
Publicar un comentario