
Sepsis Complications and Prevention
Sepsis is a condition brought on by infection of a pathogen, wherein the body reacts in such a way that it harms itself. This can be by overreacting to the infection, imbalances between the proinflammatory and anti-inflammatory responses, and the action of various mediators of the immune system.
Sepsis can be deadly, with severe complications including multiple organ failure and amputations. Despite the presence of sepsis being traced back to Roman times, sepsis is still one of the hardest conditions to treat and is responsible for thousands of hospital deaths every year.
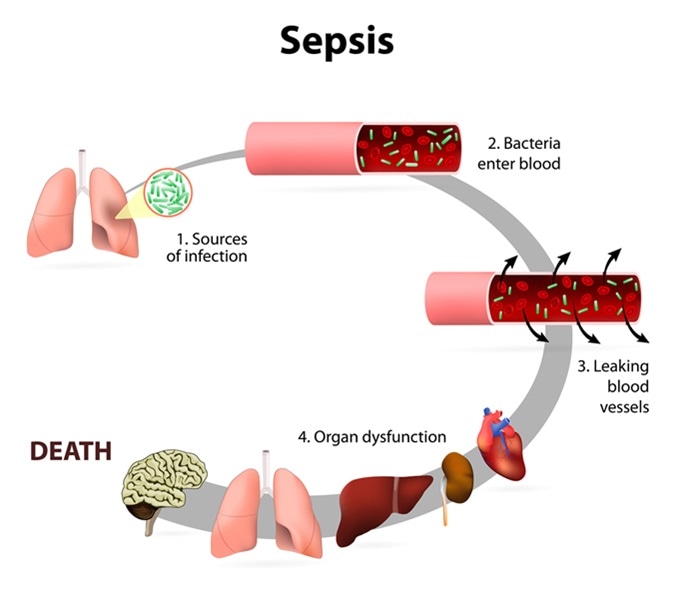
Sepsis or septicaemia is a life-threatening illness. Presence of numerous bacteria in the blood, causes the body to respond in organ dysfunction. Image Credit: Designua / Shutterstock
Severe Sepsis
There are different conditions of varying severity within the sepsis disease.. Sepsis itself is defined as known or suspected infections along with symptoms of systemic inflammatory response syndrome (SIRS). Severe sepsis is a complication of sepsis, wherein in addition to sepsis there is acute organ dysfunction. Such dysfunction can include hypoperfusion (decreased blood flow through organs) and hypotension (low blood pressure), which are commonly implicated in sepsis and severe sepsis.
Severe sepsis is the middle stage, between sepsis and septic shock. It is estimated that 20-50% of patients who develop severe sepsis die as a result. Improvements have decreased the proportional fatality rates, but the number of people dying from sepsis at any stage increases due to increased cases. Therefore, preventing sepsis is of increased focus.
Complications
The chances of developing complications of severe sepsis can depend on the type of infection and its location. Septic patients with respiratory infections are at higher risk of developing respiratory organ dysfunction, including complications such as acute respiratory distress syndrome (ARDS). The exact causes of organ dysfunction are not fully elucidated, but link partially to lack of oxygen. Impaired tissue oxygenation is caused by various factors including low blood pressure, reduced red blood cell deformability, and microvascular thrombosis. Reduced red blood cell deformability refers to the blood cell’s ability to change shape under stress without rupturing. Reduced deformability contributes to decreased stress resistance. Microvascular thrombosis refers to blood clotting, which during sepsis, occurs within blood vessels and can therefore block them.
Intracellularly, mitochondrial damage impairs oxygen use once oxygen arrives at tissues and cells. This is caused by the oxidative stress the mitochondria experiences during sepsis complication leading to severe sepsis. Injured mitochondria also release alarmins, a type of danger signal, into the extracellular environment. These alarmins can include mitochondrial DNA (mtDNA) and formyl peptides. The alarmins activate neutrophils, which cause tissue damage.
Intracellularly, mitochondrial damage impairs oxygen use once oxygen arrives at tissues and cells. This is caused by the oxidative stress the mitochondria experiences during sepsis complication leading to severe sepsis. Injured mitochondria also release alarmins, a type of danger signal, into the extracellular environment. These alarmins can include mitochondrial DNA (mtDNA) and formyl peptides. The alarmins activate neutrophils, which cause tissue damage.
In serious severe sepsis cases, the brain can be injured as a complication of sepsis. During severe sepsis the brain is often the first organ to fail and up to 70% of sepsis patients experience disturbances in brain function as a result of the immune reaction. Nitric oxide, produced during the immune reaction in sepsis, affects the brain and the aforementioned mitochondrial function. Because it is easily diffusible, it can cross the blood-brain barrier and form oxygen radicals. The following oxidative stress in brain tissue encumbers function.
Prevention
Sepsis is caused by the body’s reaction to infectious pathogens. Therefore, preventative treatment focuses on eliminating infections that would trigger that kind of reaction from your body. Basic hygiene, such as good handwashing habits and cleaning of wounds, is one of the easier courses of action. This includes using antibiotic creams or sanitizers on wounds and hands, covering wounds from exposure, and not breaking blisters.
Vaccinations against viral diseases form an effective preventative treatment against sepsis. Once a vaccination has been administered, the body has dealt with the weakened form of the virus and becomes immune. This prevents the onset of a big immune reaction if the virus is encountered again, thereby not causing the cascade leading to sepsis. Some people, such as those who are immunocompromised or allergic to vaccination ingredients, may not be able to get vaccinated against certain diseases. These will have to rely on herd immunity, where the rest of the population is vaccinated to such a degree that viral diseases cannot be carried in the population and will therefore not reach the person in question.
Other demographics are harder to protect from sepsis. Newborn babies, infected with a pathogen within one month of life, pose one such group in which prevention methods are not immediately obvious. Maternal immunization can help; however, this is often poorly advertised and not always available in poorer countries. During delivery, the cleanliness of the facility and people involved have been shown to affect occurrence of neonatal sepsis. Similarly, post delivery, the nurses and associated people’s cleanliness is important. There is some evidence suggesting cleaning of the umbilical stump with antiseptics can reduce sepsis instances, particularly in poorer settings.
Sources
Further Reading
Last Updated: Sep 14, 2018



































No hay comentarios:
Publicar un comentario