
Rogue Antibodies and Gene Mutations Explain Some Cases of Severe COVID-19
Posted on by Dr. Francis Collins
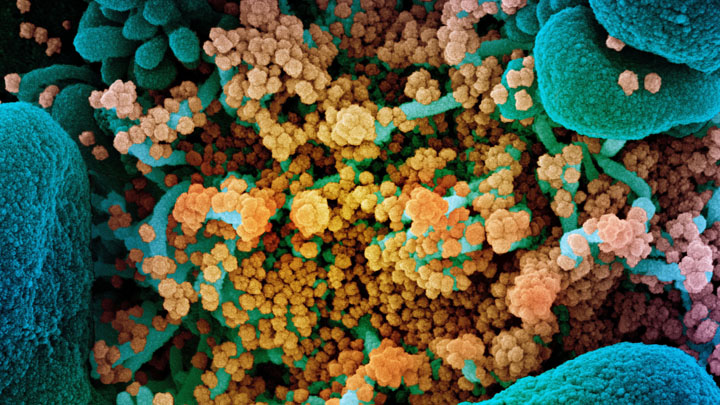
One of the many perplexing issues with COVID-19 is that it affects people so differently. That has researchers trying to explain why some folks bounce right back from the virus, or don’t even know they have it—while others become critically ill. Now, two NIH-funded studies suggest that one reason some otherwise healthy people become gravely ill may be previously unknown trouble spots in their immune systems, which hamper their ability to fight the virus.
According to the new findings in hundreds of racially diverse people with life-threatening COVID-19, a small percentage of people who suffer the most severe symptoms carry rare mutations in genes that disrupt their antiviral defenses. Another 10 percent with severe COVID-19 produce rogue “auto-antibodies,” which misguidedly disable a part of the immune system instead of attacking the virus.
Either way, the outcome is the same: the body has trouble fending off SARS-CoV-2, the novel coronavirus that causes COVID-19. The biological reason is there’s not enough of an assortment of signaling proteins, called type I interferons, that are crucial to detecting dangerous viruses like SARS-CoV-2 and sounding the alarm to prevent serious illness.
The research was led by Jean-Laurent Casanova, Howard Hughes Medical Institute and The Rockefeller University, New York; and the Imagine Institute, Necker Hospital, Paris. Casanova and his team began enrolling people with COVID-19 last February, with a particular interest in young adults battling severe illness. They were curious whether inherent weaknesses in their immune systems might explain their surprising vulnerability to the virus despite being otherwise young and healthy. Based on earlier findings in other infectious illnesses, they were especially interested in a set of 13 genes involved in interferon-driven immunity.
In their first study, published in the journal Science, researchers compared this set of genes in 659 patients with life-threatening COVID-19 to the same genes in 534 people with mild or asymptomatic COVID-19 [1]. It turned out that 23, or 3.5 percent, of people with severe COVID-19 indeed carried rare mutations in genes involved in producing antiviral interferons. Those unusual aberrations never turned up in people with milder disease. The researchers went on to show in lab studies that those genetic errors leave human cells more vulnerable to SARS-CoV-2 infection.
The discovery was certainly intriguing, but given the rarity of those mutations, it doesn’t explain most instances of severe COVID-19. Still, it did give Casanova’s team another idea. Perhaps some other people who suffer from severe COVID-19 lack interferons too, but for different reasons. Perhaps their bodies were producing rogue antibodies that were crippling their own antiviral defenses.
In their second study, also in Science, that’s exactly what researchers found in 101 of 987 (over 10 percent) patients from around the world with life-threatening COVID-19 [2]. In the bloodstreams of such individuals, they detected auto-antibodies against an assortment of interferon proteins. Those antibodies, which blocked the interferons’ antiviral activity, weren’t found in people with more mild cases of COVID-19.
Interestingly, the vast majority of patients with those harmful antibodies were men. The findings might help to explain the observation that men are at greater risk than women for developing severe COVID-19. The patients with auto-antibodies also were slightly older, with about half over the age of 65.
Many questions remain. For instance, it’s not yet clear what drives the production of those debilitating auto-antibodies. Might there be more mutations in antiviral defense-related genes that researchers have yet to discover? Is it possible that interferon treatment may help some people with severe COVID-19? Such treatment may be difficult in patients with auto-antibodies, although some clinical trials to explore this possibility already are underway.
The findings, if confirmed, have some potentially immediate implications. It’s possible that screening patients for the presence of damaging auto-antibodies might help to identify those at greater risk for progressing to severe disease. Treatments to remove those antibodies from the bloodstream or to boost antiviral defenses in other ways also may help. Ideally, it would be a good idea to make sure donated convalescent plasma now being tested in clinical trials as a treatment for severe COVID-19 doesn’t contain such disruptive auto-antibodies.
These new findings come from an international effort involving hundreds of scientists called the COVID Human Genetic Effort . Besides its ongoing efforts to understand severe COVID-19, Casanova says his team is also taking a look at the other side of the coin: how some people who’ve been exposed to severe COVID-19 in their own households manage to not get sick. A related international group called the COVID-19 Host Genetics Initiative is pursuing similar goals. Such insights will be invaluable as we continue to manage and treat COVID-19 patients in the future.
References:
[1] Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Zhang Q, Bastard P, Liu Z, Le Pen J, Moncada-Velez M, Gorochov G, Béziat V, Jouanguy E, Sancho-Shimizu V, Rice CM, Abel L, Notarangelo LD, Cobat A, Su HC, Casanova JL et al. Science. 2020 Sep 24:eabd4570. [Published online ahead of print.]
[2] Auto-antibodies against type I IFNs in patients with life-threatening COVID-19. Bastard P, Rosen LB, Zhang Q, Michailidis E, Hoffmann HH, Gorochov G, Jouanguy E, Rice CM, Cobat A, Notarangelo LD, Abel L, Su HC, Casanova JL et al. Science. 2020 Sep 24:eabd4585. [Published online ahead of print.]
Links:
Coronavirus (COVID-19) (NIH)
Interferons (Alpha, Beta) (NIH)
Interferons. Taylor MW. Viruses and Men: A History of Interactions. 2014 July 22. (Pubmed)
Video: Understanding the underlying genetics of COVID-19 , Jean-Laurent Casanova (Youtube)
Jean-Laurent Casanova (The Rockefeller University, New York)
NIH Support: National Institute of Allergy and Infectious Diseases





















.png)












No hay comentarios:
Publicar un comentario