Joint Pain and Arthritis
Chronic pain caused by arthritis affects millions of people in the United States every year. About one in four adults with arthritis—15 million people—report experiencing severe joint pain related to arthritis.1 Additionally, nearly half of adults with arthritis have persistent pain.2
Children with arthritis have pain as well, but there is less population-based information about them.
Learn about arthritis-related severe joint pain in the United States, and recommended pain management strategies that can help people with arthritis control their pain.
Defining Pain
Severe joint pain: When an individual rates his or her pain as 7 or higher out of 10 on a scale of 0 (no pain) to 10 (as bad as it can be).
Persistent pain: When an individual reports having pain (of any severity) on most or all days in the past 3 months.
Severe Joint Pain Among Adults With Arthritis
Arthritis-related severe joint pain affects adults of all ages, both sexes, and all races and ethnicities. Most of what we know about severe joint pain is for adults. The age-standardized prevalence of severe joint pain among adults with arthritis varies by state, ranging from 20% in Utah to 46% in Mississippi.1
From 2002 to 2014 in the United States, severe joint pain prevalence among adults with arthritis was:
- Higher among women (29.2%) than men (22.7%).
- Highest among adults aged 45 to 64 years (30.7%). Prevalence was the same for adults aged 18 to 44 years (24.9%) and adults aged 65 years or older (24.3%).
- Highest among non-Hispanic Blacks (42.3%), followed by Hispanics (35.8%), and non-Hispanic whites (23.1%).
Text description available.
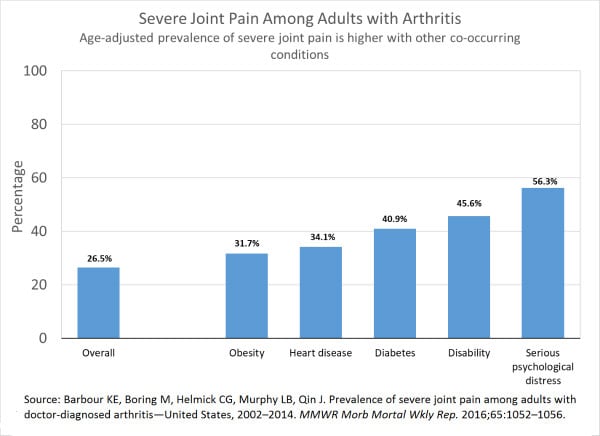
- Severe joint pain is more common among adults with arthritis who also have other chronic conditions including diabetes (40.9%), heart disease (34.1%), and obesity (31.7%), and among adults with a disability (45.6%).
- More than half (56.3%) of adults with arthritis and serious psychological distress reported having severe joint pain.
CDC’s Efforts to Reduce Arthritis Pain
CDC supports programs for people with arthritis so they can work and do other daily activities, have less pain, manage their own care, and prevent or delay disability.
CDC research related to pain includes:
- Studies examining how adults with arthritis prefer to manage their pain.
- Analyses of the effectiveness of community-based programs in reducing pain and improving quality of life.
The combined efforts and partnerships of CDC’s funded programs have made proven arthritis-appropriate self-management education workshops and physical activity intervention programs available to more than 180,000 adults in 48 states, the District of Columbia, and one territory—American Samoa. Learn more about the reach of CDC-funded Programs.
Arthritis and Joint Pain Management
Many professional organizations have guidelines for managing arthritis pain. A common theme across guidelines is that pain management strategies should be flexible, include options that do not involve medication, and be tailored to meet the needs of the patient. Such guidelines suggest the following for managing arthritis symptoms such as pain:
- Over-the-counter medications like acetaminophen (e.g., Tylenol®) or ibuprofen (e.g., Advil® or Motrin®) and other nonsteroidal anti-inflammatory drugs (NSAIDs).
- Physical activity/exercise or community-based physical activity programs.
- Exercise therapy, including physical therapy.
- Self-management education workshops.
- Weight loss, if overweight or obese.
- Cognitive behavioral therapy—a psychological, goal-directed approach in which patients learn how to modify physical, behavioral, and emotional triggers of pain and stress.
Prescription Opioids
Prescription opioids are medications that can be used to treat moderate to severe pain. Many adults with arthritis are prescribed opioids,3 but there is a lack of evidence of their long-term effectiveness when used for chronic conditions such as arthritis.
Safer options exist to help manage arthritis pain.
Over-the-Counter Medications
Emerging evidence suggests that these are safer and more effective treatments for managing long-term arthritis pain than opioids.
- A recent study of individuals with knee and hip osteoarthritis, the most common types of arthritis, found that after one year, people who took over-the-counter medications had greater reductions in pain severity than people who took opioids.4
Arthritis Pain Management without Medications
There are multiple ways for adults with arthritis to reduce their pain without using medications. In particular, CDC recommends evidence-based physical activity and self-management education programs that are proven to improve the quality of life of people with arthritis. Learn more about CDC recognized programs for managing arthritis symptoms, including pain.
Physical Activity
- Regular physical activity can help relieve adult arthritis pain as effectively as over-the counter medications.5
- Physical activity has many additional benefits, including improved physical function and mood and reduced anxiety.6
- Walking, biking, swimming, and other water activities (e.g., water aerobics, aqua jogging) are all effective ways to ease arthritis pain and are safe for most adults.
- Learn more about physical activity for arthritis.
Physical Activity Recommendations
- The 2008 Physical Activity Guidelines for Americans7 recommend:
- Two hours and 30 minutes (150 minutes) of moderate-intensity aerobic activity (i.e., brisk walking) every week. This can be broken down into smaller increments such as three, 10-minute sessions throughout the day.
- Muscle strengthening activities that work all major muscle groups (legs, hips, back, abdomen, chest, shoulders, and arms) on 2 or more days a week. In addition to pain reduction, the other arthritis-specific benefits include improved physical function and decreased disability.
- Aerobic and strengthening activities that improve balance and strengthen legs for adults aged 65 years or older to prevent falls.
Community-Based Physical Activity Programs
Community-based physical activity programs teach people how to be physically active safely and are a good option for people who are concerned about making their joint pain or arthritis worse. Physical activity programs can result in clinically important improvements in pain and function.8
CDC recommends several community-based physical activity programs that are proven to improve the quality of life of adults with arthritis. Local programs are available at YMCAs, parks, and recreation or community centers across the country.
- Learn more about CDC-recognized physical activity programs like Active Living Every Day, EnhanceFitness, Fit & Strong!, and group-based Walk With Ease.
- A promising self-directed program is also available. Participants read the Walk With Ease book, complete the exercises, and engage in walking as a way to be physically active.
Self-Management Education Workshops
Self-management education workshops teach participants life skills to reduce or manage arthritis pain and improve quality of life.
- CDC recommends adults with arthritis participate in self-management education workshops, like the Chronic Disease Self-Management Program (CDSMP), designed for people with arthritis or other chronic conditions. These workshops teach participants strategies to control or limit their symptoms, including pain, and to develop more confidence in managing health problems that affect their lives.
- Workshop participants reported significant improvements in their physical health, including less pain and increased ability to do social and household activities.
- They also noted positive changes in their mental health, including decreased depression, fear, worry, and frustration, as well as increased confidence in their ability to manage their arthritis and other chronic conditions.
- Additionally, participants also reported positive health behaviors such as increased exercise.9
- Learn more about CDC-recognized self-management education workshops.
Related Links
References
- Barbour KE, Boring M, Helmick CG, Murphy LB, Qin J. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052–1056.
- Kennedy J, Roll JM, Schraudner T, Murphy S, McPherson S. Prevalence of persistent pain in the US adult population: new data from the 2010 National Health Interview Survey. J Pain. 2014;15(10):979–984.
- Guy GP, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morbid Mortal Wkly Rep. 2017;66(26):697–704.
- Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the SPACE randomized clinical trial. JAMA. 2018;319(9):872–882.
- Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: a systematic overview of current evidence. PLoS ONE. 12(6): e0178621.
- Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18(2):189–193.
- US Department of Health and Human Services; Physical Activity Guidelines Advisory Committee (2008) Physical Activity Guidelines for Americans Website. https://health.gov/PAguidelines/. Accessed September 13, 2018.
- Kelley GA, Kelley KS, Hootman JM, Jones DL. Effects of community-deliverable exercise on pain and physical function in adults with arthritis and other rheumatic diseases: a meta-analysis. Arthritis Care Res. 2011;63(1):79–93.
- Brady TJ, Murphy L, O’Colmain BJ, et al. A meta-analysis of health status, health behaviors, and health care utilization outcomes of the Chronic Disease Self-Management Program. Prev Chron Dis. 2013;10:E07.





















.png)












No hay comentarios:
Publicar un comentario