
Life support training continues for MHS clinical staff
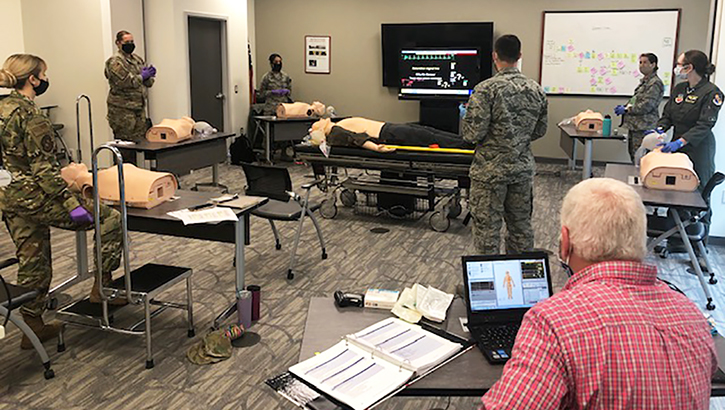
Life support instructors at Seymour Johnson Air Force Base (pictured) reduced class size to allow each trainee the recommended six feet of space in the classroom. Students rotated life saving techniques at their own stations, with a one-to-one ratio of equipment to trainee. (Air Force photo provided by Air Force Maj Sonnie Stevens, Seymour Johnson AFB.)
Life support serves as the cornerstone of medicine according to Navy Cdr. Thomas Sather, life support training manager at the Defense Health Agency. However, the close contact required for life support training made it difficult for clinical staff to keep up-to-date on training certifications while social distancing during the COVID-19 pandemic. Health care providers throughout the Military Health System accepted the challenge and found creative ways to complete this vital training.
DHA follows Centers for Disease Control and Prevention guidance for the pandemic, complete with social distancing measures whenever possible. But Sather noted that the nature of life support training involves interaction among clinical staff that could result in exposure to the virus.
“The novel coronavirus is spread through exhalation, and you can’t social distance during CPR or advanced life support,” Sather said. “We follow a ‘train as you fight, fight as you train’ philosophy. So, when you have people doing chest compressions and performing rescue breathing into a mannequin between 12 and 20 times a minute during a high stress evolution, you can see how the training may lead to some concerns.”
DHA supported military hospitals and clinics that chose to temporarily cancel basic and advanced life support training to prevent the spread of COVID-19 in their local climates. As such, DHA released guidance in March granting extensions to clinical staff whose life support training completion cards were set to expire between March and June.
Clinical staff who did not already hold certifications still needed to complete life support training before working in the field. For hospitals and clinics that continued to train, DHA guidance aligned with guidelines of the American Red Cross and the American Heart Association and created a blended or multi-modal learning environment for trainees.
“Life support is one of those key cornerstone skills needed for maintaining the life of not just the warfighter but also our beneficiaries,” Sather said. “So the very fact that we were able to continue training is just a wonderful testament to the can-do attitude of people in the military, and in particular in our MHS.”
This can-do attitude was shown at Seymour Johnson Air Force Base in Goldsboro, North Carolina. Air Force Maj. Sonnie Stevens, flight commander for group education and training at the 4th Medical Group, used a blend of online knowledge tests and hands-on experiences to keep his team current on training.
“We were getting very close to having a backlog of people whose certifications were expired,” Stevens said, “so we had to look at various ways we can conduct the training and do it safely.”
Trainees completed their knowledge tests through online resources from the American Red Cross. Stevens then reduced class size to allow each trainee the recommended 6 feet of social distancing space in the classroom. Students rotated life-saving techniques at their own stations, with a one-to-one ratio of equipment to trainee. Stevens noted that the distance was actually helpful for training.
“Communication is critical with this new class construct, because there is added distance which requires participants to speak louder. The students also had to be intentional about monitoring the actions of others,” Stevens said. “I think it enhanced participation and the awareness during the training.”
The MHS requirement for clinical staff to recertify in life support certifications resumes in July. Clinical staff whose certifications have expired have 120 days from the expiration date to complete their training. With updated life support training guidance from the American Red Cross, Stevens embraced the changes and encourages others to do the same.
“Think outside the box because we are developing a new norm,” Stevens said, “You have to look at training in a new light and seize opportunities to make sure that you provide a service and maintain safety.”
As for Sather, he is confident that MHS hospitals and staff remain ready to perform and adjust to the ever-changing environment of COVID-19.
“The mission of the Defense Health Agency is to support and provide medical care to the warfighter and our medical patients,” Sather said. “It's very encouraging to know that our staff will continue to deliver high-quality care, even during these trying times.”
Applying COVID-19 innovations to the future of MHS medicine
Article
7/14/2020

COVID-19 has already irrevocably changed how we deliver care and will continue to do so.
U.S. military deploys to Texas and California in support of COVID-19 operations
Article
7/14/2020

[A]pproximately 740 Department of Defense medical and support professionals from the Army, Navy and Air Force deployed to support COVID-19 operations in Texas and California.
COVID-19 Asymptomatic Testing Clinic opens at NMRTC Bremerton
Article
7/13/2020

[S]tanding up the CAT clinic will assist in identifying asymptomatic COVID-positive individuals and assist the continual effort to stop the spread of the pandemic.
Convalescent Plasma Donation PSA featuring Lt. General Place
Video
7/10/2020

Lt. Gen Place asks servicemembers DoD-wide to consider dontating plasma in the fight against COVID-19.
For some, working from home brings neck and back pain
Article
7/10/2020

"[T]he most common complaint of teleworkers is neck and upper back pain between the shoulder blades."
DHA's new app assists providers with treating infectious diseases
Article
7/10/2020

This progressive web application provides faster updates to content and function than traditional apps.
New Invention Helps Protect Healthcare Workers During COVID-19 Pandemic
Article
7/9/2020

"[T]he team realized that while the CAMIC would function well for tracheostomy, its true use would be for intubation..."
Defending the Homeland: Fort Knox Safety Official Donates COVID-19 Convalescent Plasma to Help Others
Article
7/8/2020

[T]he process involves a machine that uses three bags to collect and separate the plasma from the blood.
Summer’s here – stay safe!
Article
7/8/2020

Remember these tips while enjoying the summer
Combat stress techniques help military providers during COVID pandemic
Article
7/6/2020

6 steps to get medical team members back in the fight
Pentagon leaders brief department's COVID-19 response to reporters
Article
7/2/2020

The COVID-19 pandemic affects each area of the nation differently. Local leaders at military installations decide protocols for public safety on a case-by-case basis. The Military Health System supports those leaders by providing health surveillance data, updated to reflect current information.
Confronting the Coronavirus and Countering Complacency
Article
7/2/2020

Call it the COVID-19 complacency conundrum.
U.S. Naval Hospital Guam Collects Convalescent Plasma from Sailors
Article
7/2/2020
.ashx?h=68&la=en&mw=120&w=120&hash=0B5A7CC2C0FF6A6ED4927F1CA04D78C26FD98BD868607C5947D4B87BBCEA9905)
The CCP is the liquid part of blood from patients who have recovered from an infection.
BAMC Change of Command 2020
Article
7/1/2020

Army Brig. Gen. (Dr.) Wendy Harter, the first female commander in Brooke Army Medical Center’s history, turned over command to Army Brig. Gen. (Dr.) Shan Bagby, the first African American commander in BAMC’s history during a June 26 change of command ceremony at Joint Base San Antonio-Fort Sam Houston, Texas.
COVID-19 leads to innovation in military health care practices
Article
7/1/2020

MHS thinks outside of the box to bring care to patients during pandemic





















.png)












No hay comentarios:
Publicar un comentario