
MHS mental health experts shed light on PTSD

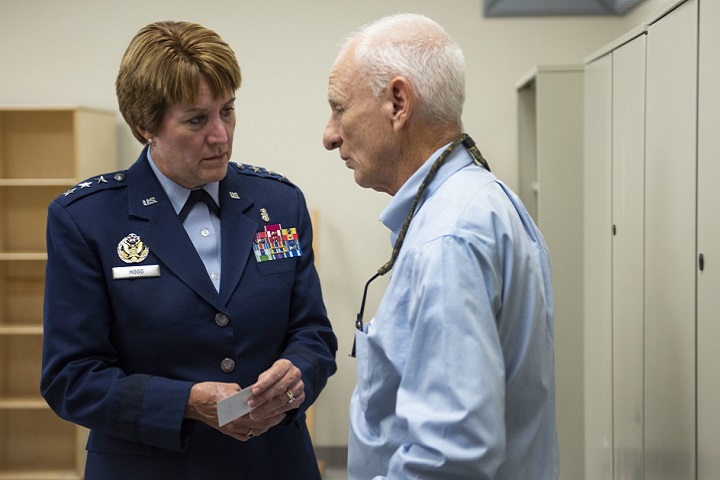
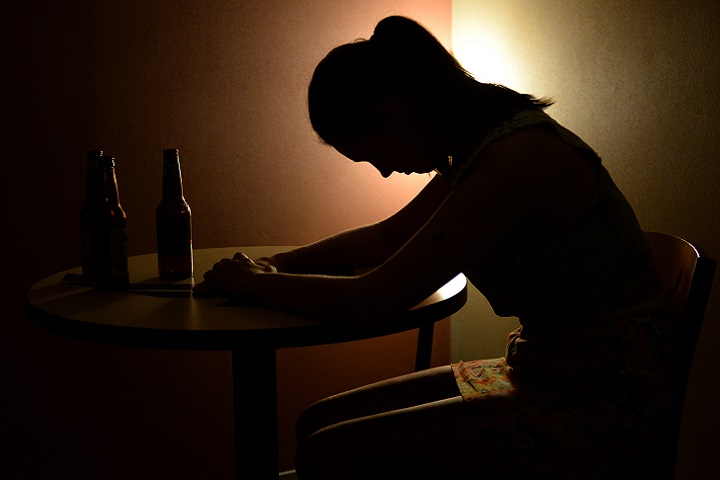
Three Military Health System mental health subject matter experts spoke Thursday during a PTSD media roundtable. It was held to recognize June as PTSD Awareness Month, and to showcase MHS programs and resources connected to PTSD treatment. (U.S. Air Force photo illustration By Senior Airman Erica Fowler)
Post-traumatic stress disorder can be treated long after the triggering event occurs, three Military Health System mental health subject matter experts said Thursday. But all agree getting help as soon as possible avoids health issues that can occur as a result of living with PTSD. And effective psychotherapy treatments are available now, even if people can't meet with providers face to face because of pandemic restrictions.
The experts' comments came during a PTSD media roundtable by telephone. It was held to recognize June as PTSD Awareness Month, and to showcase MHS programs and resources connected to PTSD treatment.
The three experts answering reporters' questions were David Riggs, Ph.D., executive director of the Center for Deployment Psychology at Uniformed Services University of the Health Sciences in Bethesda, Maryland; Dr. Robert Ursano, director of USU's Center for the Study of Traumatic Stress; and Public Health Service Lt. Cmdr. Jorielle Houston, Ph.D., clinical psychologist with the Psychological Health Center of Excellence.
PTSD is a mental health condition that can develop after exposure to traumatic events such as threat of injury or death, serious accident, combat, terrorist attack, sexual assault, physical assault, natural disaster, and childhood sexual or physical abuse.
Many individuals with PTSD repeatedly re-experience the traumatic event as flashback episodes, memories, nightmares, or frightening thoughts, especially when exposed to events that remind them of the trauma.
"Over a lifetime, nearly everybody is exposed to a traumatic event," Ursano said. However, not everyone develops PTSD. Variables that put people at risk for it include prior trauma history, lack of social support, suffering an injury as a result of the trauma, and pre-existing mental health issues.
"Mental health has common colds as well as cancers, and PTSD can be both," Ursano said, adding that "the vast number of people …with PTSD are on a recovery trajectory."
The COVID-19 pandemic may be particularly challenging for people with PTSD, Ursano explained. Patients may be feeling an increased sense of isolation, greater irritability, and more conflict with loved ones.
With the challenges of doing face-to-face therapy during physical distancing, "I think it's important for folks to know that … [effective psychotherapies] are able to be delivered using telehealth technologies," Riggs said.
He noted that during the past few months, Department of Defense clinics have seen a decrease in demand for PTSD treatment. This aligns with an overall decreased access to health care during the pandemic, he said.
"When you delay care, you increase your risk" for more severe health issues, he said.
Houston noted that PHCoE seeks social media channels to highlight evidence-based practices including exposure, cognitive processing, and stress inoculation therapies.
Riggs said DoD clinics are "already planning and anticipating the potential increase" after physical distancing rules are lifted, and they expect telehealth use also will increase.
"Some of the clinics are finding that patients actually prefer that option to coming in," he said. "In terms of figuring out how to handle potential or possible increase in demand, it's figuring out how to balance the use of resources for in-person appointments as opposed to telehealth appointments."
In response to a question about whether the proper medical term should be PTSD or post traumatic stress, Houston said she was "more concerned about, how do we figure out what is going on with the symptoms, and the root of the symptoms, than … the label. How do we get service members the help they need? How do we get the family members the help they need? How do we get providers the support they need?"
Houston mentioned DoD initiatives including the Real Warriors and Make the Connection campaigns, which encourage service members to ask for help and recognize that seeking help is a sign of strength. Resources for family members include Military OneSource and Military Kids Connect, which offers age-appropriate resources to support children dealing with the unique psychological challenges of military life.
"We want to continue to spread the message that those who suffer from the fallout of traumatic experiences … are not alone," Houston said. And it doesn't matter if the trauma is related to combat, disease, domestic strife, or personal tragedy, she said.
"You do not need to suffer in silence. There is help. There is comfort. There is hope."
The Language of Anger and Depression Among Patients with Concussions
Article
6/4/2020

Soldiers often do not overtly express their feelings of depression.
Positive attitude, social support may promote TBI/PTSD resilience
Article
7/23/2019

Psychological experiences prior to an injury may play a role in recovery
Warm Handoff for Transitioning Servicemembers Suffering from PTSD and TBI
Congressional Testimony
7/8/2019
S. 2987, SASC Report for FY 2019, 115-262, Pg. 203-204
Pilot Program on Treatment of Members of the Armed Forces for PTSD Related to Military Sexual Trauma
Congressional Testimony
6/10/2019
H.R. 5515 NDAA Report for FY 2019, Sec. 702
Pilot Program on Investigational Treatment of Members of the Armed Forces for TBI and PTSD
Congressional Testimony
10/9/2018
HR 3304, NDAA for FY 2014, Sec. 704
PTSD Trigger Record
Fact Sheet
9/27/2018
Trigger Records can help you recognize what situations are triggering your PTSD
PTSD Trauma Triggers and Memories Overview
Fact Sheet
9/27/2018
An overview of what trauma triggers are and how they can impact those with PTSD
Air Force's first Invisible Wounds Center opens
Article
9/10/2018
The center will serve as a regional treatment center for post-traumatic stress, traumatic brain injury, associated pain conditions and psychological injuries
Drug-monitoring innovations help providers help their patients
Article
8/6/2018
Focus is on management of pain and PTSD
Seizures among Active Component service members, U.S. Armed Forces, 2007 – 2016
Infographic
1/25/2018

This infographic documents a retrospective study which estimated the rates of seizures diagnosed among deployed and non-deployed service members to identify factors associated with seizures and determine if seizure rates differed in deployment settings. The study also evaluated the associations between seizures, traumatic brain injury (TBI), and post-traumatic stress disorder (PTSD) by assessing correlations between the incidence rates of seizures and prior diagnoses of TBI and PTSD.
DCOE Annual Report 2014
Report
7/16/2015
Annual Report for the Defense Center of Excellence - 2014
Guidance for Providers Prescribing Atypical Antipsychotic Medication 12-003
Policy
Articles in popular media, and the concern of several national and military leaders in recent months, have raised the question of whether certain psychoactive medications are inappropriately prescribed for post-traumatic stress disorder (PTSD) and commonly comorbid conditions.
- Identification #: 12-003
- Date: 2/22/2012
- Type: Memorandums
- Topics: Posttraumatic Stress Disorder





















.png)












No hay comentarios:
Publicar un comentario