
Coronavirus: What you need to know
A Guardsmen with the 341st Military Intelligence Battalion conducts translation work on a safety message regarding the best practices for avoiding the novel coronavirus for the Washington Department of Health on Feb. 9, 2020 at the Information Operations Readiness Center, Joint Base Lewis-McChord, Wash. (Courtesy Photo)
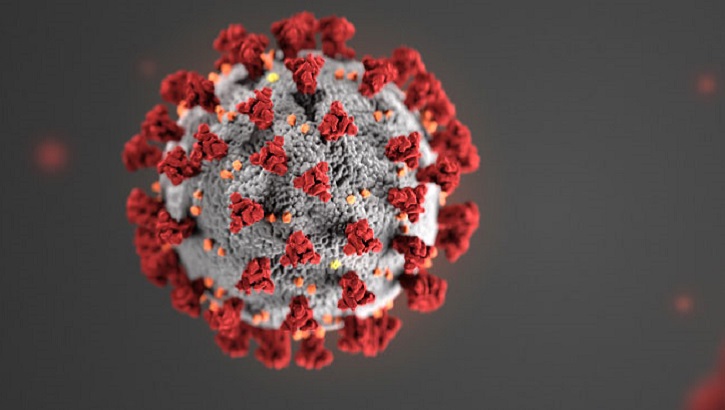
JOINT BASE LEWIS-McCHORD, Wash. -- Novel coronavirus, known as COVID-19, continues to spread worldwide.
As COVID-19 spreads, so does information about the disease. If one surfs the Internet, everything from scientifically-proven medical information about the virus to debunked conspiracy theories can be found.
More than 95,000 cases have been reported worldwide, and COVID-19 has killed more than 3,300 people, mostly in mainland China.
The disease has spread wider in Washington state, where ten people have died. A 71-year-old-man in California with underlying health conditions passed away from the disease this week, bringing the nationwide death total to 11.
Washington Gov. Jay Inslee declared a state of emergency on Feb. 29, a number of school districts have cancelled classes, and more than 50 people in a Seattle-area nursing facility are being tested for the virus.
According to the Centers for Disease Control, there were 205 confirmed cases of COVID-19 in the U.S. as of March 5. The disease has spread to 17 U.S. states. The Washington State Department of Health reported 70 cases in the state as of March 5.
Among the information circulating online are lists of items people "should buy" -- surgical masks, exam gloves, gallons of disinfectant -- but epidemiologists and preventive medicine practitioners say that's not exactly the case.
While there is currently no vaccine to protect against COVID-19 and no specific antiviral treatment for the disease, Lt. Gen. Ronald J. Place, director of the Defense Health Agency, stated in a March 5 email to the force that "Each of you can take actions to help respond to this emerging public health threat."
Place's email also stated, "The CDC has produced more than 23 guidance documents on infection control, hospital preparedness assessments, personal protective equipment supply planning, and clinical evaluation and management."
According to the CDC, symptoms of COVID-19 can include fever, cough, and shortness of breath. The CDC believes that symptoms of the disease may appear in as little as two days or up to 14 days after someone has been exposed.
The CDC based this estimate on previous incubation periods for Middle East Respiratory Syndrome, another type of coronavirus, first reported in 2012.
The CDC said there are simple actions people can take to prevent contracting or spreading COVID-19.
The best way to keep from getting sick, according to the CDC, is to avoid being exposed to the virus that causes COVID-19.
The Department of Defense issued guidance in January, mirroring that of the CDC. The DoD guidance recommended that people should also avoid close contact with those who are sick; avoid touching your eyes, nose and mouth with unwashed hands; and washing your hands often with soap and water.
The CDC recommends washing hands for at least 20 seconds, especially after going to the bathroom, before eating, after blowing one's nose, coughing or sneezing.
Although news stories and images contain many reports of people wearing surgical masks to ward off the virus, that's not recommended, according to top officials of the U.S. Public Health Service.
The U.S. Surgeon General, Dr. Jerome Adams, even went so far as to post a message on Twitter last weekend.
"Seriously people- STOP BUYING MASKS!" Jerome tweeted. "They are NOT effective in preventing general public from catching #Coronavirus, but if healthcare providers can't get them to care for sick patients, it puts them and our communities at risk!"
The CDC and DoD also recommend using an alcohol-based hand sanitizer that is at least 60 percent alcohol if soap and water aren't available.
The spread of coronavirus has led to a shortage of hand sanitizers and disinfectants in stores, and Army and Air Force Exchange Service locations haven't been spared.
Chris Ward, senior public affairs manager at AAFES headquarters in Dallas, said in an email that the entire supply chain for hand sanitizer products and masks has been severely constrained.
"Like other retailers, the Exchange has experienced shortages of hygiene items due to a surge in demand due to COVID-19," the email stated.
Ward's email went on to state that AAFES is "aggressively working to procure additional inventory to expedite shipment to locations impacted by COVID-19," and recommended following the CDC guidance stating that hand washing is the best defense to preventing the spread of infection.
But what if someone contracts COVID-19? What should they do?
Above all, said the CDC, anyone sick with COVID-19, or if one suspects they are infected, should follow these steps:
- Stay home, except to get medical care: Restrict activities outside your home, except for getting medical care. Do not go to work, school, or public areas. Avoid using public transportation, ride-sharing, or taxis.
- Separate yourself from other people and animals in your home: As much as possible, stay in a specific room and away from other people in the home. Also, use a separate bathroom, if available.
- Call ahead before visiting your doctor: Call the healthcare provider and tell them that you have or may have COVID-19. This will help the healthcare provider's office take steps to keep other people from getting infected or exposed.
- Cover your coughs and sneezes: Cover your mouth and nose with a tissue when you cough or sneeze. Throw used tissues in a lined trash can. Immediately wash your hands with soap and water for at least 20 seconds.
- Clean your hands often: Wash your hands often with soap and water for at least 20 seconds, especially after blowing your nose, coughing, or sneezing; going to the bathroom; and before eating or preparing food.
- Avoid sharing personal household items: Don't share dishes, drinking glasses, cups, eating utensils, towels, or bedding with other people or pets in your home. After using these items, they should be washed thoroughly with soap and water.
- Clean all "high-touch" surfaces every day: High touch surfaces include counters, tabletops, doorknobs, bathroom fixtures, toilets, phones, keyboards, tablets, and bedside tables. Also, clean any surfaces that may have blood, stool, or body fluids on them. Use a household cleaning spray or wipe, according to the label instructions.
- Monitor your symptoms: Seek prompt medical attention if your illness is worsening, such as if you have difficulty breathing). Before seeking care, call your healthcare provider and tell them that you have, or are being evaluated for, COVID-19.
The CDC also said that those patients with confirmed COVID-19 should remain under home isolation precautions until the risk of secondary transmission to others is thought to be low. The decision to discontinue home isolation precautions should be made on a case-by-case basis, in consultation with healthcare providers and state and local health departments.
For the most up-to-date information on COVID-19, visit the CDC's website. Specific Military Health System information about COVID-19 can be found at health.mil/News/In-the-Spotlight/Coronavirus.
Epidemiology lab supports flu vaccine development
Article
2/11/2020
The lab shares information with the CDC and helps push potential changes to the influenza vaccine each year
MHS prepared to support interagency coronavirus response
Article
2/6/2020

From R&D to force health protection, MHS protects DoD personnel and families
MSMR Vol. 27 No. 2 - February 2020
Report
2/1/2020
A monthly publication of the Armed Forces Health Surveillance Branch. This issue of the peer-reviewed journal contains the following articles: Update: Malaria, U.S. Armed Forces, 2019; Diabetes mellitus and gestational diabetes, active and reserve component service members and dependents, 2008–2018; Increased risk for stress fractures and delayed healing with NSAID receipt, U.S. Armed Forces, 2014–2018; Brief report: Diagnoses of scarlet fever in Military Health System (MHS) beneficiaries under 17 years of age across the MHS and in England, 2013–2018; Images in health surveillance: Skin rashes in children due to infectious causes
DoD releases guidance to protect forces from novel coronavirus
Article
1/31/2020
Basic infection controls offer best defense against illness
Coronavirus: What providers, patients should know
Article
1/24/2020
What to do now that virus has appeared in U.S.
DTRA contributes to historic Ebola vaccine effort
Article
1/17/2020
U.S. Food and Drug Administration approves new Ebola vaccine
MSMR Vol. 27 No. 1 - January 2020
Report
1/1/2020
A monthly publication of the Armed Forces Health Surveillance Branch. This issue of the peer-reviewed journal contains the following articles: Carbon Monoxide Poisoning, Active and Reserve Component Service Members and Non-Service Member Beneficiaries of the Military Health System, U.S. Armed Forces, July 2009–June 2019; Respiratory Pathogen Surveillance Trends and Influenza Vaccine Effectiveness Estimates for the 2018–2019 Season Among Department of Defense Beneficiaries; Brief Report: The Early Impact of the MHS GENESIS Electronic Health Record System on the Capture of Healthcare Data for the Defense Medical Surveillance System; and Brief Report: Incidence and Prevalence of Idiopathic Corneal Ectasias, Active Component, 2001–2018.
Air Force International Health Specialist builds medical capability in Iraq
Article
12/30/2019

Cowden’s work facilitated the exchange of medical knowledge and practices between Kurdish and Iraqi security forces.
Global Health Engagement strengthens partnerships
Article
12/20/2019
.ashx?h=68&la=en&mw=120&w=120&hash=EFEB174C823214FB196EAB6A1BDA54165C083899FA1B8379BCC5E324DA381782)
GHE advances U.S. national security interests around the world
Ship-based Global Health Engagement
Article
12/4/2019

Global health engagement is an important priority for military medicine
Network of researchers advancing warfighter readiness
Article
12/4/2019

In fiscal year 2020, GEIS awarded approximately $60 million to more than 20 DoD laboratories and U.S. government partners
World AIDS Day puts spotlight on landmark DoD study
Article
12/2/2019
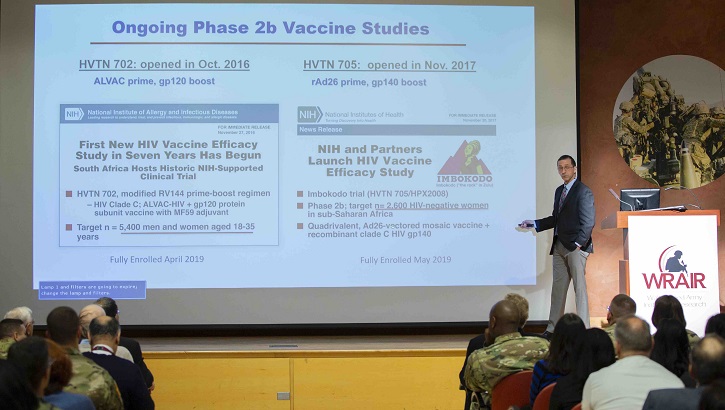
Vaccine study shows infection risk lowered by 31 percent, offering hope for future
MSMR Vol. 26 No. 12 - December 2019
Report
12/1/2019
A monthly publication of the Armed Forces Health Surveillance Branch. This issue of the peer-reviewed journal contains the following articles: Editorial: Mitigating the risk of disease from tick-borne encephalitis in U.S. military populations; Tick-borne encephalitis surveillance in U.S. military service members and beneficiaries, 2006–2018; Case report: Tick-borne encephalitis virus infection in beneficiaries of the U.S. military healthcare system in southern Germany; Update: Cold weather injuries, active and reserve components, U.S. Armed Forces, July 2014–June 2019
Antibiotic resistance a serious threat that's growing, CDC warns
Article
11/15/2019

Newly published paper outlines issue, offers possible solutions
USNS Comfort strengthens partnership with Jamaica
Article
11/7/2019

This marks the Comfort’s third visit to Jamaica





















.png)












No hay comentarios:
Publicar un comentario