Childhood Acute Lymphoblastic Leukemia Treatment (PDQ®)–Health Professional Version
General Information About Childhood Acute Lymphoblastic Leukemia (ALL)
Cancer in children and adolescents is rare, although the overall incidence of childhood cancer, including ALL, has been slowly increasing since 1975.[1] Dramatic improvements in survival have been achieved in children and adolescents with cancer.[1-3] Between 1975 and 2010, childhood cancer mortality decreased by more than 50%.[1-3] For ALL, the 5-year survival rate has increased over the same time from 60% to approximately 90% for children younger than 15 years and from 28% to more than 75% for adolescents aged 15 to 19 years.[4] Childhood and adolescent cancer survivors require close monitoring because cancer therapy side effects may persist or develop months or years after treatment. (Refer to the PDQ summary on Late Effects of Treatment for Childhood Cancer for specific information about the incidence, type, and monitoring of late effects in childhood and adolescent cancer survivors.)
Incidence
ALL is the most common cancer diagnosed in children and represents approximately 25% of cancer diagnoses among children younger than 15 years.[2,3] In the United States, ALL occurs at an annual rate of approximately 41 cases per 1 million people aged 0 to 14 years and approximately 17 cases per 1 million people aged 15 to 19 years.[4] There are approximately 3,100 children and adolescents younger than 20 years diagnosed with ALL each year in the United States.[5] Since 1975, there has been a gradual increase in the incidence of ALL.[4,6]
A sharp peak in ALL incidence is observed among children aged 2 to 3 years (>90 cases per 1 million per year), with rates decreasing to fewer than 30 cases per 1 million by age 8 years.[2,3] The incidence of ALL among children aged 2 to 3 years is approximately fourfold greater than that for infants and is likewise fourfold to fivefold greater than that for children aged 10 years and older.[2,3]
Anatomy
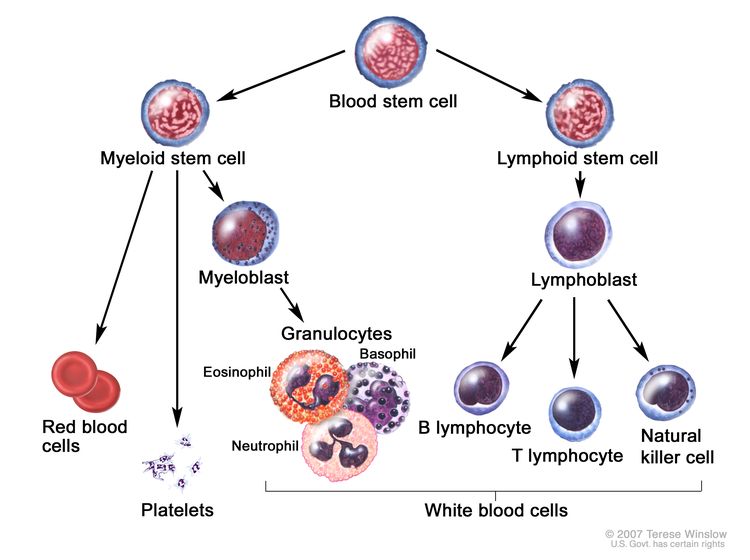
Childhood ALL originates in the T and B lymphoblasts in the bone marrow (refer to Figure 1).
Marrow involvement of acute leukemia as seen by light microscopy is defined as follows:
- M1: Fewer than 5% blast cells.
- M2: 5% to 25% blast cells.
- M3: Greater than 25% blast cells.
Almost all patients with ALL present with an M3 marrow.
Morphology
In the past, ALL lymphoblasts were classified using the French-American-British (FAB) criteria as having L1 morphology, L2 morphology, or L3 morphology.[9] However, because of the lack of independent prognostic significance and the subjective nature of this classification system, it is no longer used.
Most cases of ALL that show L3 morphology express surface immunoglobulin (Ig) and have a MYC gene translocation identical to those seen in Burkitt lymphoma (i.e., t(8;14)(q24;q32), t(2;8)) that join MYC to one of the Ig genes. Patients with this specific rare form of leukemia (mature B-cell or Burkitt leukemia) should be treated according to protocols for Burkitt lymphoma. (Refer to the PDQ summary on Childhood Non-Hodgkin Lymphoma Treatment for more information about the treatment of mature B-cell lymphoma/leukemia and Burkitt lymphoma/leukemia.) Rarely, blasts with L1/L2 (not L3) morphology will express surface Ig.[10] These patients should be treated in the same way as are patients with B-ALL.[10]





















.png)












No hay comentarios:
Publicar un comentario